Let’s talk about your second brain.
There is a living, dynamic universe within you. A biological ecosystem so sophisticated that it influences everything from your mood and metabolism to your immune system and mental health. It is a pillar of wellness that scientists are only beginning to understand. That understanding will potentially revolutionize how we think about human health.
Every second of every day, trillions of microscopic bacteria, fungi, and other microorganisms are dancing around in this internal universe. These vast communities of microbes (primarily residing in your large intestine), form what scientists call . . .
THE GUT MICROBIOME.
What was once considered solely digestion is now recognized as a complex and highly synchronized internal world essential to physical health and mental wellness.
The gut’s microbial community is so vast, complex, and influential that it essentially behaves as its own autonomous organ—a second brain, if you will.
This topic can be dense and is often discussed using technical biological terms. While much of the research is generally consistent, some discrepancies exist across various studies. Our aim is to distill and present the information as clearly and accurately as possible.
HOW THE GUT MICROBIOME WORKS
By now, you’ve likely heard the phrase “gut microbiome” quite a bit. Perhaps you know about probiotics and maybe even prebiotics. Even without knowing exactly what it is or how it works, you know the gut microbiome is important.
Here are some wild facts you should know about the gut:
- There are more bacterial cells in your body than human cells (40 trillion vs. 30 trillion).
- There are at least 1,000 distinct species of bacteria (likely much more) living in the gut. Each performs different tasks in the body. Not all bacteria are bad.
- The gut microbiome weighs approximately 2-5 lbs (about the weight of a pineapple).
- Around 90% of the body's serotonin, our body’s “happy” chemical, is produced in the gut.
- Your gut contains significantly more neurons than your spinal cord
- About 70-80% of the body’s immune cells are located in your gut’s lymphoid tissue and interact with your microbiome.
Understanding how the gut microbiome affects your health requires exploring three fundamental areas of influence: metabolism, immunity, and the gut-brain connection.
Metabolism
Your gut microbes transform the food you eat into energy and compounds your body can use. They break down fiber into short-chain fatty acids, which nourish your intestinal cells, regulate inflammation, improve insulin sensitivity, and regulate blood sugar levels. Our gut bacteria produce several essential vitamins that our bodies cannot synthesize on their own. The primary vitamins produced include vitamin K and various B vitamins.
Immune System Function
Your gut microbiome is a sophisticated training ground for your immune system. From birth, microbes help immune cells distinguish between what's friendly and what's dangerous. Our earliest exposure to microbes—through vaginal delivery, breast milk, and skin-to-skin contact—help set up our immune system’s baseline.
About 70–80% of the body’s immune cells reside in the gut wall, where they maintain the gut barrier, prevent “leaky gut,” and determine what to attack. Leaky gut occurs when the gut barrier becomes permeable, allowing harmful substances into the bloodstream. This triggers something called endotoxemia, a series of inflammatory responses throughout the body.
The relationship between microbes and immunity is so fundamental that scientists now believe many modern immune disorders, allergies, and chronic inflammation may stem from disrupted microbial communities.
THE GUT–BRAIN CONNECTION
"How is it that the bugs in your gut are connected to obesity, diabetes, cancer, heart disease, dementia, autism, autoimmune disease, allergies, asthma, depression? I could go on and on. Everything is connected to the microbiome. How does that make sense given our paradigm? If you are going to your psychiatrist with depression, are they saying, let me look at your poop? Well, they should, okay, literally they should. I've literally cured people of the worst psychiatric conditions you can imagine by fixing their gut."
—Dr. Mark Hyman, Eudēmonia Summit 2024
So why do they call it your second brain? For three main reasons:
- The gut and brain are connected through neural, hormonal, and immune pathways, with a superhighway called the vagus nerve as a key component in the bidirectional relationship between these organs. (We may have to dedicate a future newsletter just to the vagus nerve. It’s that fascinating.)
- Second, your gut has its own nervous system, called the enteric nervous system (ENS). It’s often referred to as the “second brain” because it can operate independently of our first brain. It’s an autonomous and self-sustained system, and the ENS has many of the same neurons and neurotransmitters that our first brain has.
- Third, and maybe most important, is the neurochemical influence, by which the gut microbiome can profoundly influence our mental and emotional health. Because of the gut–brain axis, emotional and cognitive centers of the brain are directly linked to intestinal functions. This helps explain why digestive health often correlates with mental health.
Research has shown that microbiome disruptions may contribute to anxiety, depression, and even neurodegenerative conditions. Conversely, psychological stress can alter your gut microbiome, creating a feedback loop between mind and microbes. The connection is so strong that scientists have found that transplanting gut bacteria from people with depression into healthy rats can actually make the rats exhibit depressive behaviors. And studies have shown that people with depression or anxiety often have a less diverse microbiome.
In short, a healthy gut could trigger better moods and better brain function.
WHAT INFLUENCES YOUR MICROBIOME
Your gut microbiome is shaped by a complex interplay of factors—from the food you eat to the environment you live in—working together to influence your overall health and well-being.
Diet
Insufficient fiber and excessive consumption of highly refined carbohydrates, processed foods, and refined sugars are among the most common gut disruptors. What you eat has such a profound impact on your gut that your microbes can respond rapidly to dietary changes, often within 24-48 hours. However, establishing a stable and healthy microbiome composition requires consistent, healthy dietary habits.
Lifestyle
Chronic stress and poor sleep have a negative impact on your gut microbiome, as does a sedentary lifestyle that doesn’t prioritize regular exercise.
Medications
Heavy reliance on certain prescription drugs like NSAIDs, statins, and painkillers all contribute to gut dysregulation. Antibiotics can be particularly detrimental, as they significantly alter the gut microbiome by killing both harmful and beneficial bacteria indiscriminately.
Enviroment
Everything from where you live, the cleaning products you use, and the air you breathe has an impact. The chemicals, pollutants, and pesticides you’re exposed to all influence the stability of your microbiome.
Early Life
Vaginal birth, breast milk, and avoiding early exposure to antibiotics positively shape your initial microbiome.
THE DANGERS OF AN UNHEALTHY GUT
Gut imbalance can manifest in surprising ways, affecting not just digestion but your immune system, mood, skin, energy levels, and more. Here are some key warning signs to watch for.
- Digestive Issues: irregular bowel movements, bloating, gas or abdominal discomfort, acid reflux, or heartburn
- Immune System Issues: recurring infections, slow wound healing, frequent colds, severe seasonal or food allergies, chronic inflammation
- Cognitive Signs: mood changes, brain fog, increased anxiety or depression, irritability
- Skin Problems: acne, eczema, rosacea, dry or itchy skin, rashes
- Unusual Fatigue: low energy that doesn’t improve with rest, difficulty sleeping
- Food Sensitivities: new sensitivities to previously tolerated foods, gluten or dairy intolerance emerging
- Hormonal Indicators: irregular menstrual cycles, PMS symptoms worsening, weight fluctuation
It cannot be overstated how important a healthy gut microbiome is to your overall wellness. Disruptions in gut microbiota and gut permeability have been connected to both the causes and effects of a wide range of conditions and diseases, some of which may surprise you.
COVID-19
Research has shown that COVID-19 patients exhibit significant alterations in gut microbiota composition, including reduced bacterial diversity and depletion of beneficial bacteria. This gut dysbiosis may contribute to disease severity and persistence of symptoms in long COVID. Studies have also found that a healthy, diverse microbiome might help protect against severe COVID-19 outcomes and support recovery.
Neurological Conditions
- Autism Spectrum Disorder: Studies have found that children with autism often exhibit gut microbial dysbiosis, which may play a role in the development of the condition.
- Parkinson’s Disease: Studies show that individuals with PD demonstrate a wide imbalance in bacterial composition, overproduction of toxic molecules, and dysregulation of neurotransmitters, linking the disease to issues in the GI tract.
- Alzheimer’s Disease: Recent studies reveal a strong connection between Alzheimer’s Disease and the gut microbiome. Researchers discovered that people in the early stages of the disease exhibit distinct gut bacteria profiles, even before experiencing noticeable cognitive decline. These differences in gut microbiota are associated with brain changes and inflammation linked to Alzheimer’s Disease.
- Attention Deficit Hyperactive Disorder (ADHD): Studies have shown that individuals with ADHD often have different gut microbiome compositions compared to those without ADHD.
Metabolic Conditions
- Obesity: Some gut microbes produce obesity-promoting metabolites and certain gut bacteria may be more efficient at extracting energy from food, potentially contributing to weight gain. Studies have found distinct differences between the gut microbiomes of lean and obese individuals.
- Type 2 Diabetes: Altered gut microbiota affects glucose metabolism, insulin sensitivity, and inflammation, increasing risk for diabetes. Research shows that specific bacterial strains may either protect against or promote diabetes development.
Cardiovascular Health
- Cardiovascular Disease: The gut microbiome plays a crucial role in regulating cholesterol metabolism and inflammation, both of which are key contributors to heart disease.
- Hypertension: Gut microbiota has been found to influence blood pressure by producing compounds that affect blood vessel function.
Digestive Conditions
- Colon Cancer: Specific bacterial patterns and metabolites produced by gut bacteria may increase colon cancer risk. These metabolites can create an environment that increases susceptibility to carcinogenic stimuli.
- Irritable Bowel Syndrome (IBS): Microbiome imbalances are now recognized as a key factor in the development and symptom severity of IBS. This has led to increased interest in microbiome-targeted therapies—such as probiotics, prebiotics, and fecal microbiota transplantation—as potential treatment options for managing IBS symptoms.
ANALYZING THAT GUT FEELING
Several companies offer comprehensive at-home tests for analyzing the gut microbiome.
- Verisana Comprehensive Gut Biome & Health Test
This test examines various aspects of gut health using stool samples. - ZOE Microbiome Test
This test uses both stool and blood samples to provide a comprehensive analysis. - GI Effects Comprehensive Profile by Genova Diagnostics
This test assesses complete gut health by analyzing your stool.
You can also contact a gastroenterologist or functional medicine practitioner to do these tests for you.
HOW TO ACHIEVE GUT ENLIGHTMENT
So what can we do to nurture our gut health and support a balanced microbiome?
01. Eat the Rainbow
Food is mood. This might sound ambitious, but research from the American Gut Project suggests aiming to eat 30 different plant foods weekly. Each color represents different compounds that feed diverse bacterial communities. Focus on fruits, vegetables, tubers, whole grains, nuts, seeds, and legumes.
This will also get you lots of fiber, which is very important for colon health. A recent study found that higher total dietary fiber intake was associated with a significantly reduced risk of colon cancer. As a rule, aim for 30g of fiber per day.
02. Include Fermented Foods
Fermented foods promote and add healthy bacteria to your gut. These foods include yogurt with live cultures, kombucha, kimchi, sauerkraut, tempeh, pickles in brine, sourdough bread, and miso.
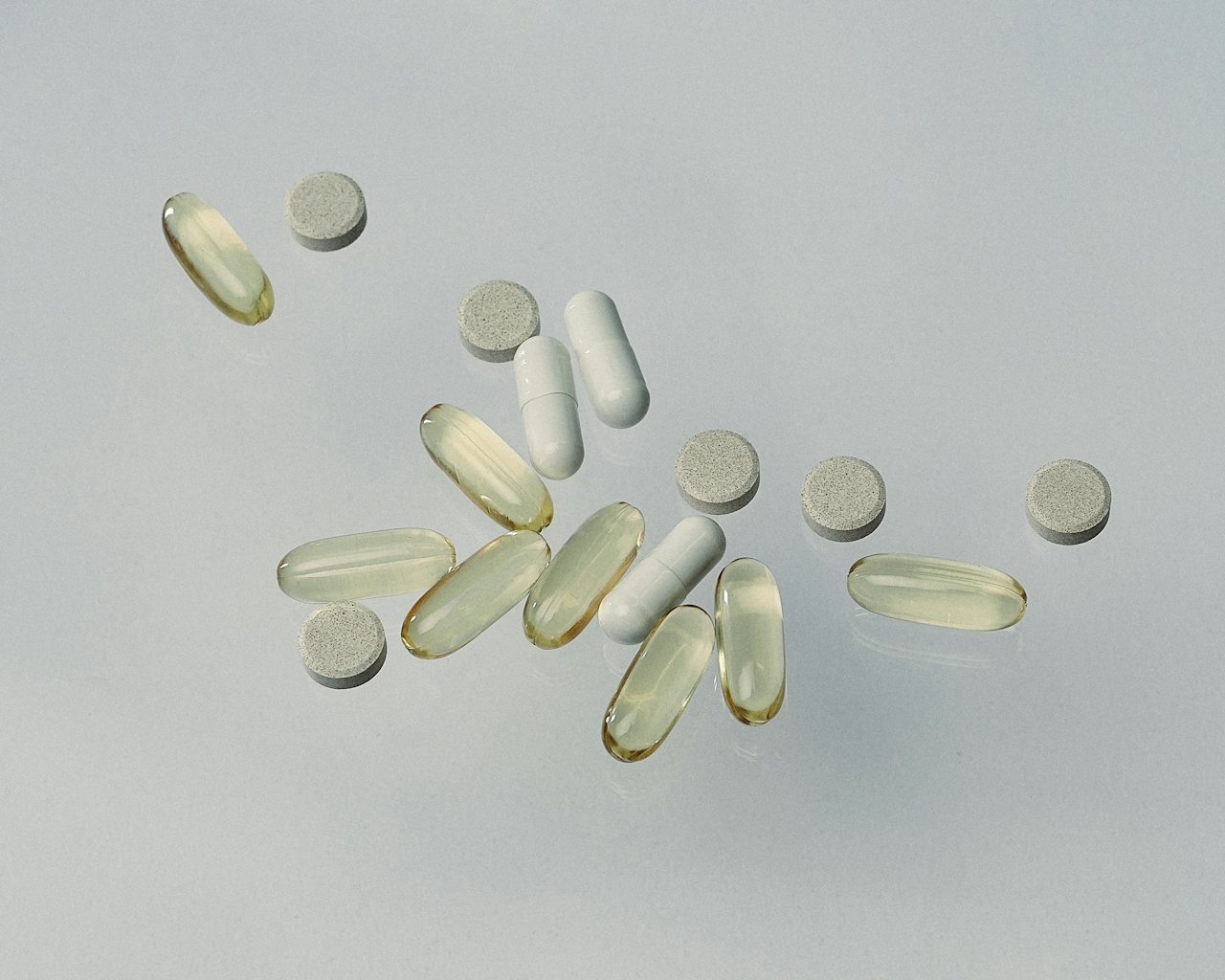
03. Incorporate Probiotics and Prebiotics
Probiotics are “good” bacteria that live in and promote a healthy gut, and are found in the fermented foods listed above. Prebiotics are fibers from plants that serve as food for the probiotics in your gut. We want a diet that includes both, but there are also ways to supplement these.
04. Avoid Sugar and Processed Food
This is ubiquitous health advice, but it is important to mention that excess sugar and processed foods can promote the growth of harmful bacteria and cause inflammation. In particular, foods high in artificial sweeteners and emulsifiers can alter microbial populations and intestinal barriers.
05. Drink Plenty of Water
Staying hydrated helps maintain the gut’s protective barrier, which aids in preventing conditions like leaky gut.
06. Manage Stress
Stress does all kinds of wacky things to your gut. It impacts digestion, harms the gut’s protective lining (leading to leaky gut), and disrupts the communication of gut-brain axis, which can lead to mental health issues. Regularly practicing meditation, yoga, or anything else that relieves stress in a healthy way is important.
07. Exercise
Aerobic work, strength training, and restorative movement all promote microbial diversity and enhance gut barrier function. Incorporating a balance of brisk walking or jogging or cycling, yoga or pilates, and strength training is a good regimen for a healthy gut—and a generally healthy life.
Incorporating a 10-minute walk after meals has been shown to reduce blood sugar levels up to 35%. Stable blood sugar is important for maintaining a healthy gut microbiome, and it lowers stress and reduces gas and bloating.
08. Spend Time In Nature
Gardening exposes you to a diverse range of microorganisms through your skin, which can support immune function and improve mood. Plus, time outdoors increases vitamin D levels through exposure to sunlight, which also supports gut barrier integrity.
STRATEGIC SUPPLEMENTATION
A diet that prioritizes a wide range of plants and incorporates fermented foods should be your primary focus...
...but there have been many developments in supplementation that can support gut health, and there are many companies making great products.
Before experimenting, you should always consult with a doctor and consider getting tested to understand the health of your gut.
When choosing supplemental probiotics, select products with multiple strains and rotate brands periodically to introduce different beneficial species. Also, certain strains may aid in digestive health, while others might support immune function. Consult a healthcare professional to identify the strain best suited to your health needs, as effects vary from person to person.
You can also consider introducing supplemental prebiotics, but start slowly to avoid digestive discomfort. Some use natural antimicrobial compounds like oregano oil or berberine occasionally to help maintain microbial balance. Finally, Vitamin D may increase microbial diversity, helps regulate intestinal barrier integrity, and supports immune function in the gut.
EMERGING TRENDS IN GUT HEALTH
Exciting new treatments and technologies are emerging that could revolutionize how we approach gut health and overall wellness.
Fecal Microbiota Transplantation
The procedure involves transferring processed stool from a healthy donor into the colon of a recipient to restore healthy gut bacteria.
Precision Probiotics
This concept is being actively researched, although it's still in early stages. It uses genetically engineered probiotics for tailored interventions based on individual characteristics and needs.
Microbiome Mapping
Advanced sequencing technologies are used to map individual gut microbiomes. The development of AI-powered platforms for personalized recommendations is an active area of research and commercial development.
Smart Monitoring
Wearable technologies are offering unprecedented insights into digestive system functioning with non-invasive gut health tracking.
GETTING TO THE BOTTOM OF IT ALL
Simply put, our mental health and physical well-being is dependent on a well-functioning, balanced, and diverse microbiome. It’s our second brain, and nurturing this internal ecosystem is one of the most powerful investments we can make into our long-term health.
That health is a direct reflection of our lifestyle, environment, and choices. By supporting this invisible ecosystem, we’re investing in our overall health and well-being in ways that science is only beginning to understand.
As you embark on your journey to optimize your gut health, remember that your microbiome responds best to consistent, nurturing care. Small, daily choices accumulate to create sustainable habits and significant changes. Listen to your body, stay curious about new research, and approach this complex internal world with curiosity and patience.
|
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

February 20, 2026

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026