This issue of the Eudēmonia Newsletter is independent editorial content and has not been reviewed or endorsed by any sponsor.
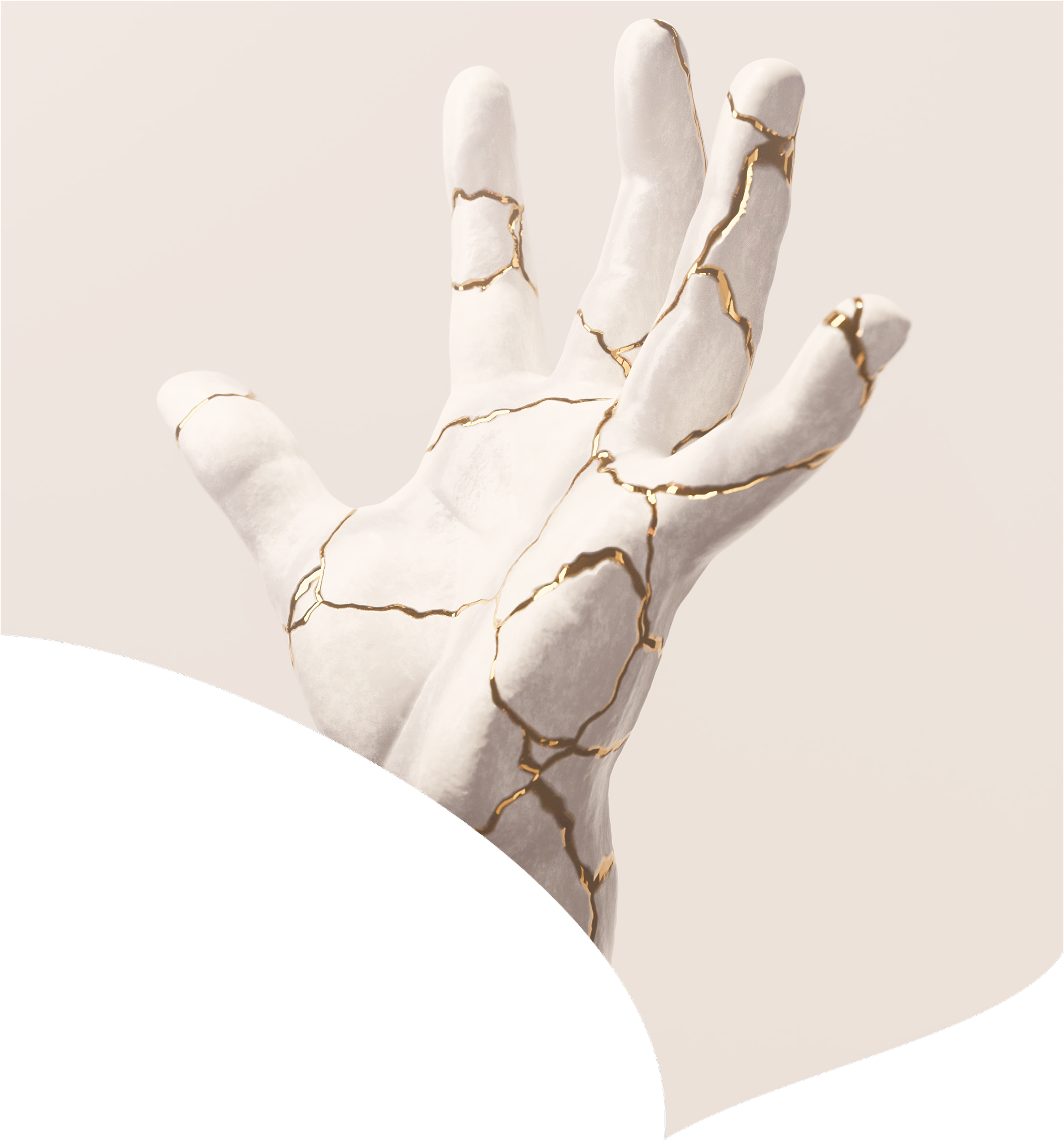
There’s a humbling math that emerges in middle age. The same training that once put you in great shape now barely maintains the status quo. The workout that left you energized at 30 leaves you depleted at 45. The soreness that cleared in 24 hours now lingers for 3 days. And the cumulative effect of work stress, poor sleep, and life demands compounds in ways it simply didn’t a decade earlier.
This isn’t a failure of discipline or effort. It’s a shift in the fundamental equation. Where output once determined outcomes, recovery capacity now becomes the bottleneck. You can maintain motivation, optimize your training program, dial in your nutrition, and still find yourself treading water simply because your body can’t repair and adapt at the rate it once could.
This reality has created an entire category (and business vertical) of recovery science and technology that barely existed ten years ago. We’re talking about a systematic approach to recovery that's become essential for anyone wanting to maintain function, preserve muscle mass, keep metabolic health intact, and prevent the gradual decline that becomes exponential without intervention.
The paradigm has shifted. Recovery isn't about bouncing back to do more. It's about maintaining the capacity to keep doing anything at all.
We won’t be going into the more obvious recovery modalities, like flexibility, mobility, and diet, all of which are fundamental to recovery, longevity, and feeling good. Instead, today’s issue focuses on the deeper systems that decide whether your body can actually stay in the fight.
The Science of Recovery: What’s Actually Happening
To understand why recovery becomes harder and what we can do about it, we need to understand what recovery actually is at a physiological level. It’s not simply the absence of stress or exertion. It’s a distinct set of biological processes that must actively occur for adaptation and repair to happen.
At the center of recovery sits the autonomic nervous system. The sympathetic branch governs stress response: fight-or-flight. The parasympathetic branch governs rest-and-digest where repair occurs.
Recovery isn’t just about time spent resting. It’s about flexibly switching between these states. The problem with age and chronic stress? This switching becomes sluggish. You get stuck in sympathetic overdrive, unable to shift into restoration.
This shows up in heart rate variability (HRV). Research in large adult cohorts shows that heart rate variability tends to decline progressively with age after early adulthood, with steeper reductions often seen in later decades, consistent with reduced autonomic flexibility.
Inflammatory resolution also slows. Research on exercise-induced muscle damage shows that older adults exhibit a slower recovery of inflammatory markers, strength, and soreness compared with younger adults. Unresolved inflammation accumulates—called allostatic load. Each new stressor adds to the existing burden rather than wiping the slate clean. You operate from a permanently elevated baseline of inflammation and sympathetic tone.
The adaptations you're seeking—muscle protein synthesis, mitochondrial biogenesis, neural strengthening—don't happen during the workout. They happen during recovery. Exercise is the signal. Recovery is when the work gets done. When recovery capacity diminishes, you're sending signals your body increasingly can't act on.
Why Recovery Becomes the Bottleneck
Understanding the mechanisms helps, but it doesn’t capture the lived experience of watching your recovery capacity erode. The “treading water” feeling has specific physiological explanations.
After about age 40, several hormonal shifts converge. Growth hormone secretion declines by roughly 15% per decade of adult life, and in men, total testosterone falls gradually by around 0.3–0.5% per year, with free testosterone declining by about 1% or more per year as sex hormone–binding globulin rises. These hormones play important roles in supporting muscle protein synthesis, tissue repair, and recovery from exercise, so their age‑related decline can contribute to slower recovery, not just reduced performance
Sleep architecture changes dramatically. Deep slow‑wave sleep, which supports physical restoration and recovery, declines markedly with age, and by the 70s some individuals have lost well over half of the deep sleep they had in early adulthood, with very little slow‑wave sleep remaining on average.
Muscle protein synthesis becomes less efficient—called anabolic resistance. Older adults need substantially more protein per meal to achieve the same muscle-building response as younger individuals. Your recovery demands increase precisely when capacity decreases.
Check Out Our Issue On Protein
Most significantly, the margin for error shrinks. At 25, you could skip sleep, eat poorly, overtrain, and bounce back within days. At 45, that same combination might require weeks to recover from or trigger an injury that lasts months. Recovery stops being automatic and becomes something you must actively create and protect.
This isn't pessimistic; it's realistic. The goal isn’t to perform like we did at 25. It's to maintain function, preserve muscle mass, and prevent the decline that becomes exponential when recovery is consistently compromised.
The Most Effective Recovery Modalities
Contrast Therapy
Contrast therapy—alternating hot and cold exposure—offers the broadest research-backed recovery benefits. Heat causes vasodilation and cold causes vasoconstriction, creating a vascular pumping effect that clears metabolic waste and reduces inflammation.
Cold exposure triggers 200–300% increases in norepinephrine, providing anti-inflammatory effects and improved focus. Sauna provides cardiovascular conditioning and increases heat shock proteins crucial for cellular repair. A 2015 study following 2,300 Finnish men found those using saunas 4-7 times weekly had 40% lower all-cause mortality.
The combination significantly reduces muscle soreness and accelerates recovery compared to passive rest.
Biochemist and peptide expert Nick Andrews recommends this thermal reset protocol:
- Step 1: Hot immersion
Sit in 110 degree water for 5 minutes. Let your muscles loosen and your breathing slow. - Step 2: Cold immersion
Move straight into 45 degree water for 5 minutes. Stay calm and steady. Let the shock settle into control.
Repeat this cycle between 110 and 45 degree water three times. Each round lasts 10 minutes. - Step 3: Sauna finish
After the third round, go into a 180 degree sauna for 15 minutes. This is the part that wipes out stress and sends HRV soaring. You come out feeling like a million bucks.
That’s the whole sequence. Three hot to cold cycles, then the long sauna.
Check Out Our Expert Q&A On Heat and Cold Therapy
Breathwork for Nervous System Regulation
Breathwork represents perhaps the most underutilized recovery tool available because it requires no equipment, no subscription, and no dedicated space. It works anywhere, anytime, and it can shift physiological state in minutes. The barrier isn’t access; it’s awareness and consistent practice.
The mechanism is straightforward: your breathing pattern directly controls your nervous system state. Rapid, shallow mouth breathing activates stress mode. Slow, deep nasal breathing with a longer exhale activates recovery mode.
Here's how it works: The vagus nerve runs from your brain to your organs and has sensors in your lungs. When you breathe slowly and deeply, these sensors trigger a relaxation response. When you extend your exhale, you activate what's called the “vagal brake”—the mechanism that slows your heart rate. If you're wearing a heart rate monitor, you can literally watch your heart rate drop in real-time as you breathe this way.
And it doesn’t take much time. Just a few minutes, or a few cycles of breath can help.
Check Out Our Issue on Meditation and Breathwork
Sound and Vibration
Sound as recovery sits between ancient wisdom and cutting-edge neuroscience. Sound baths tap into centuries of intuition about rhythm and resonance, while modern labs study frequency-specific interventions with far more precision. The challenge is separating legitimate mechanisms from hype.
The core principle is entrainment—your brain’s electrical rhythms synchronizing with external stimuli. Binaural beats, which present slightly different frequencies to each ear, have shown measurable effects in controlled studies. Theta ranges are associated with deeper relaxation. Delta ranges can support sleep quality.
Forty-hertz stimulation is even more intriguing. MIT researchers found that exposing animals to synchronized 40 Hz light and sound enhanced brain clearance mechanisms and improved cognitive markers. Early human studies are small but encouraging.
Vagus-nerve-targeted vibration adds a direct physiological lever. Several devices use vibration at the ear canal, chest, or throat to activate parasympathetic pathways and raise HRV.
Check Out Our Issue on the Vagus Nerve
Where things get powerful is pairing the sound with the vibration and layering in a modality like breathwork. Together, these stimuli reinforce one another and help the nervous system shift out of stress mode and into recovery mode. The combination can drive meaningful physiological change without wandering into claims the science can’t support.
Safety note: Generally safe, but avoid vagal nerve stimulation devices if you have cardiac issues or implanted devices.
Light Therapy
Light therapy has evolved from treating seasonal depression to a comprehensive recovery tool. Different wavelengths, intensities, and timing produce entirely different effects.
Circadian Optimization
Outdoor morning light (within 30 minutes of waking) shifts your circadian clock earlier, improving nighttime sleep and alertness. The intensity matters: indoor lighting delivers 100-300 lux while outdoor morning light provides 10,000+ lux. This is why opening blinds doesn't match stepping outside. Research shows morning exposure to high-intensity light significantly improves sleep quality, decreases depression, and boosts vitality.
Circadian Amplitude
Circadian amplitude is the strength of your day–night rhythm—how pronounced the difference between your peak alertness during the day and your deepest sleep at night is.
Think of it like a wave: high amplitude means a big swing between wide awake during the day and deeply asleep at night. Low amplitude means a flattened wave—less distinction between your daytime and nighttime states.
As we age, this amplitude decreases. The rhythm weakens. Older adults don't get as deeply asleep at night and may not feel as energetically alert during the day. This shows up as waking up earlier than you'd like, waking multiple times during the night, and generally lighter, less restorative sleep.
Bright morning light helps by giving a powerful daytime signal that reinforces the day/night distinction—essentially strengthening that wave again.
Evening Light Management
This is equally critical. Blue wavelength light (from LED screens) potently suppresses melatonin. Experimental studies show that a few hours of evening use of light‑emitting screens can suppress melatonin by around 50–60% and delay both melatonin onset and sleep onset, sometimes by up to an hour or more in susceptible individuals, especially when the devices are used in the hour or two before bedtime. The most effective intervention: reduce overall light intensity 2–3 hours before bed.
Red Light
Red and near-infrared light therapy works through photobiomodulation—a process where specific wavelengths of light penetrate your tissue and directly enhance how your cells produce energy.
Near-infrared light (810–850 nm) penetrates several centimeters, reaching muscle and bone. Red light (630–670 nm) penetrates several millimeters, affecting skin and surface tissue. When these wavelengths hit your mitochondria, they're absorbed by cytochrome c oxidase, an enzyme in the energy production pathway. This enhances ATP production, meaning your cells generate more energy and perform repair functions more effectively.
The effects are measurable. Research found photobiomodulation significantly reduced muscle fatigue and accelerated post-exercise recovery—improved strength return, reduced soreness, faster power output restoration. This is direct cellular-level enhancement, not placebo.
Applications extend beyond athletic recovery: improved muscle strength in older adults, accelerated wound healing, reduced inflammation, and benefits for chronic joint pain and tendinitis. Some emerging research suggests cognitive benefits through enhanced cerebral blood flow.
How Hormones Play Into Recovery
All of the recovery modalities we’ve discussed operate on top of a more fundamental layer: systemic physiology. Hormones are major regulators of recovery capacity, and age‑related shifts in testosterone, growth hormone/IGF‑1, thyroid hormones, and—in women—estrogen and progesterone are important reasons why bouncing back tends to get harder after midlife, alongside changes in muscle quality, sleep, and overall health.
These hormones influence muscle protein synthesis, tissue repair, sleep quality, inflammatory signaling, and metabolic function, so when they are frankly low or clearly out of range for good health, recovery is happening on a less favorable biological backdrop. In those situations, cold plunges or red‑light therapy cannot fully compensate for a significant hormonal deficit, although they may still add incremental benefit.
For women, the menopausal transition often brings abrupt hormonal changes that contribute to muscle loss, sleep fragmentation, and slower recovery, and appropriately prescribed hormone therapy can substantially improve symptoms and support musculoskeletal and metabolic health in many patients, within an individualized risk–benefit framework.
So why doesn't everyone optimize their hormones? Because it's complicated, medically intensive, and carries legitimate risks. Testosterone replacement requires ongoing monitoring and can affect cardiovascular health and prostate function. Hormone replacement for women has its own risk–benefit considerations. Growth hormone therapy is expensive, requires daily injections, and has side effects. All of these interventions require physician supervision and aren't appropriate for everyone.
Hormones set your baseline recovery capacity. Everything else maximizes what that baseline can deliver. If your hormones are significantly suboptimal, you're trying to optimize a compromised system.
Physicians in the longevity space like Peter Attia and Andrew Huberman have spoken openly about considering or using hormone replacement.
The reality is that if you've optimized fundamentals, implemented strategic recovery practices, track metrics consistently, and still experience significant recovery deficits, then comprehensive hormone assessment should be your next step. Hormones are probably the biggest variable. The cold plunge helps. The breathwork matters. But they're supporting players to the hormonal foundation.
Stay in the Game
Recovery isn't resignation; it's the prerequisite for preventing decline. The maintenance you’re doing now is what allows you to keep training, keep pushing, keep improving in select areas rather than declining across the board.
You're buying capacity. The capacity to train without injury. To handle stress without burnout. To sleep well and wake up recovered. To maintain muscle mass, metabolic health, and cognitive function as you age.
Start with the fundamentals:
- Morning light exposure
- Evening light restriction
- Basic breathwork
These three interventions alone, done consistently, produce measurable improvements within 2-4 weeks. Then add modalities based on your needs—contrast therapy for training, red light for tissue issues, evening protocols for stress and sleep.
Twenty minutes of intentional recovery daily beats two hours once a week. Make it systematic enough to become automatic, integrated into your routine like training and nutrition.
The alternative is slow-motion decline that accelerates over time. You push through depleted. Performance drops. Injuries accumulate. Sleep degrades.
Eventually you can't push anymore, because there's nothing left to push with.
Recovery is what allows you to keep playing the long game. It's not dramatic, but it works.
Build the system now. Measure what matters. Adapt as you age. And stay in the game.
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026

January 2, 2026