Every breath you take, every move you make—it all starts with mitochondria.
In the last issue, we broke down how these cellular engines decide whether you’ve got energy in the tank, how fast you recover, and how well you age.
Missed it? You can catch up on The Mitochondria Issue.
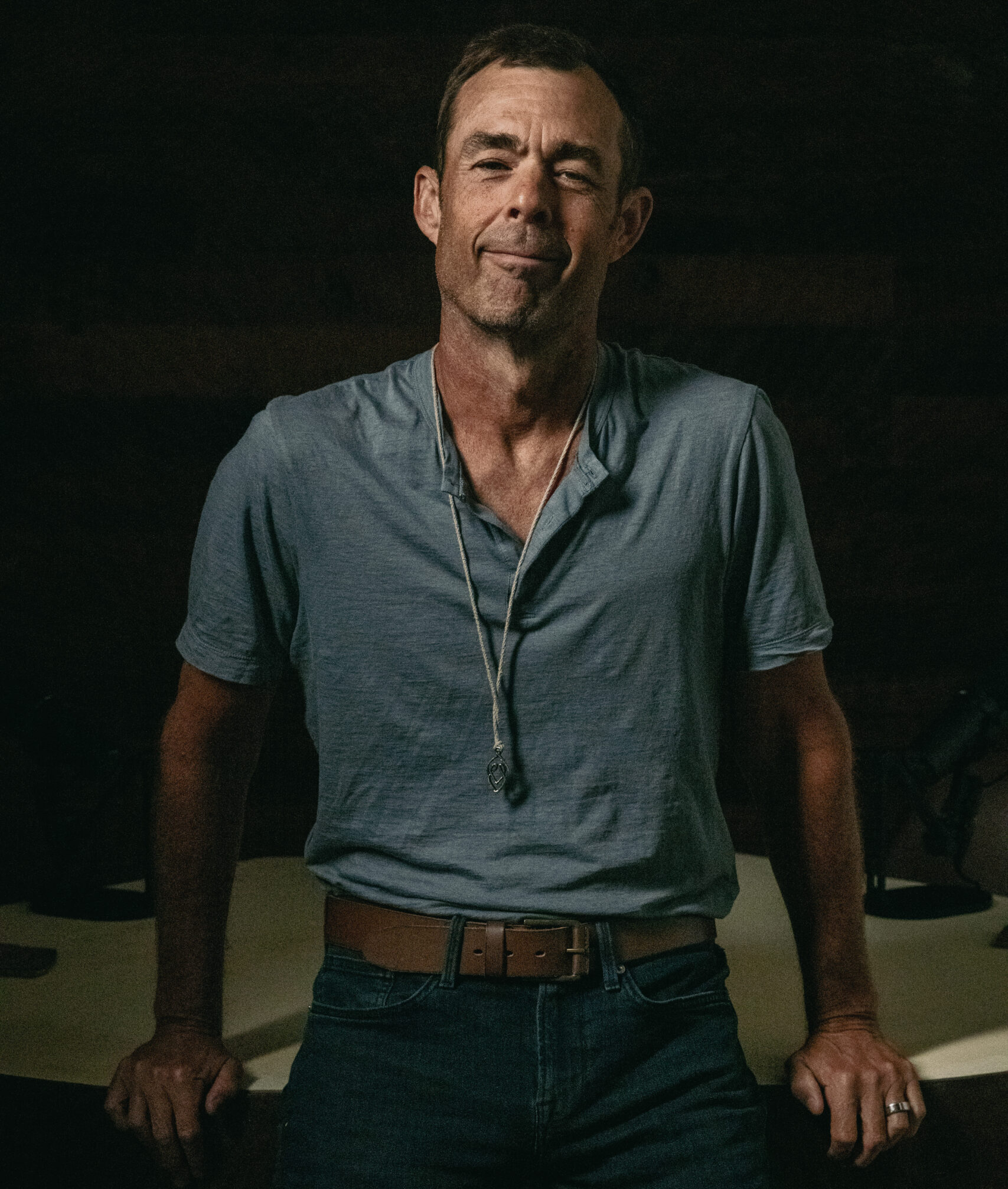
Now, Dr. Christopher Palmer is here to connect the dots between mitochondrial health, energy, and mental well-being.
Dr. Christopher Palmer is a Harvard psychiatrist and researcher who has spent decades studying the intersection of metabolism, mitochondria, and mental health. His pioneering work—outlined in Brain Energy—proposes that mental disorders are metabolic disorders of the brain. He is now launching MH², a revolutionary new model of integrated mental and metabolic health care that brings this science into clinical practice.
Let’s get into his answers to some of your biggest questions.
Q. Have you personally seen evidence linking mitochondrial dysfunction to mental health disorders like depression or anxiety? How do you determine that? And how do you treat that?
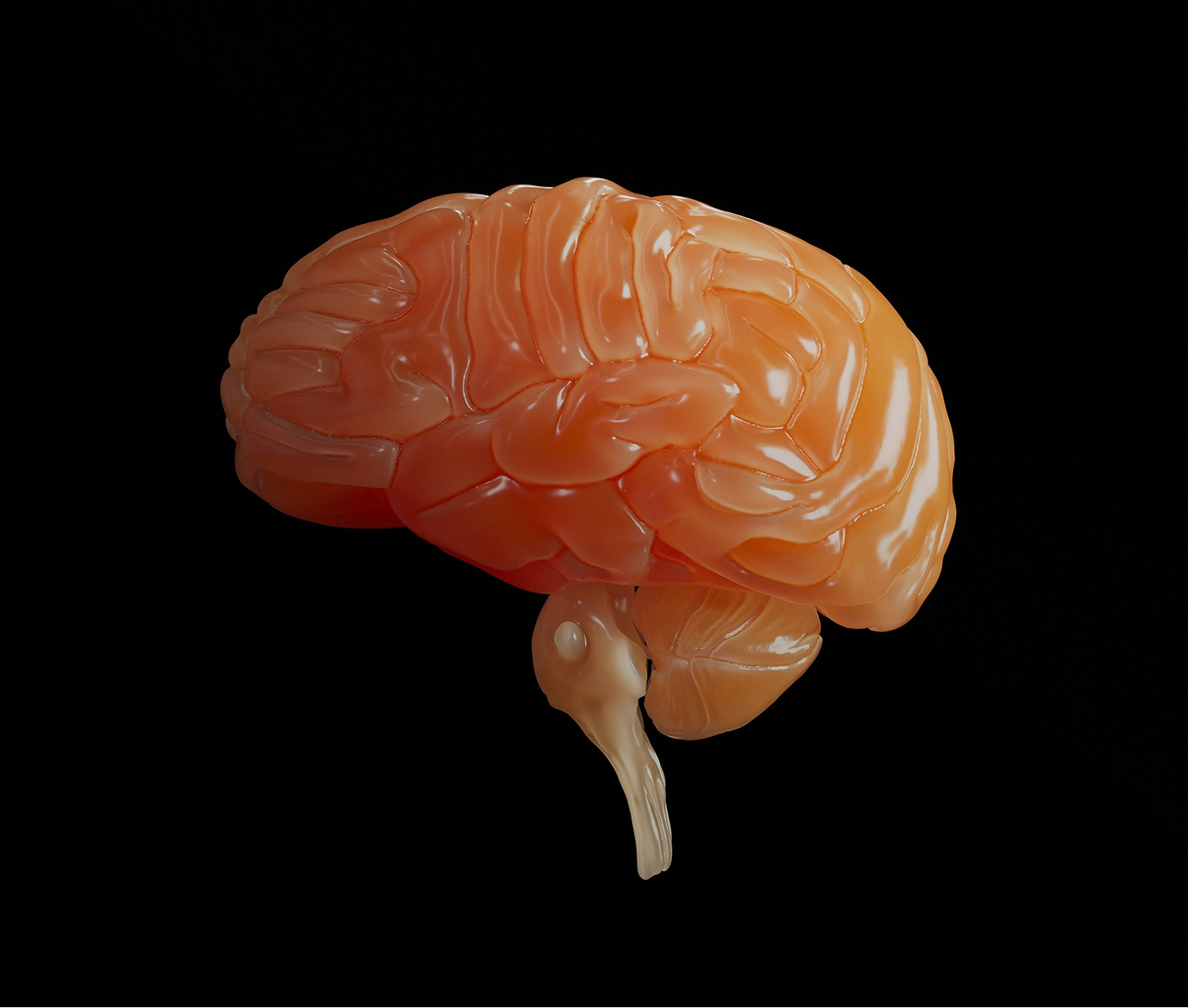
There is a substantial and growing body of scientific evidence linking mitochondrial dysfunction to mental health disorders, such as depression and anxiety. For example, brain imaging studies show elevated lactate and reduced high-energy metabolites, suggesting inefficient energy production. Postmortem analyses of the brains of people with depression and many other mental health conditions reveal reduced mitochondrial density, altered structure, and changes in mitochondrial DNA, while blood studies consistently find impaired mitochondrial respiration, lower acetyl-L-carnitine, and increased oxidative stress. Genetic and transcriptomic studies identify mitochondrial pathways as among the most dysregulated in depression and other mental
health conditions. Animal models confirm that disrupting mitochondrial function produces depression-like behaviors, while treatments that enhance mitochondrial health can improve mood.
In clinical practice, however, most of these studies aren’t readily available, so we measure things that can be easily and inexpensively measured and look for behavioral manifestations of impaired mitochondrial function. These can include signs and symptoms like fatigue, exercise intolerance, brain fog, insulin resistance, abnormal lipids (high triglycerides and low HDL), high blood pressure, elevated inflammatory biomarkers, increased levels of visceral fat, etc.
Treating mitochondrial dysfunction is complex, as there can be many different biological,
psychological, social, and environmental causes of it. The first step is trying to determine the root causes and addressing them directly.
In some people, this could include addressing an unhealthy diet, improving sleep quality, optimizing nutrients, or reducing harmful substance use, such as tobacco or alcohol. All of these lifestyle factors are known to directly impact mitochondrial function. For others, the root causes can be more complicated, such as the lingering effects of an infection, as we see in some cases of Lyme disease or Long COVID. In
these situations, we might use anti-inflammatory diets, supplements, and specific vitamins to improve mitochondrial health.
Q. Do you encourage proactive mitochondrial health? If so, what does sustained mitochondrial health look like?
Yes. Prevention is always easier than trying to fix problems once they’ve taken root. Sustained mitochondrial health shows up in many tangible ways of good health: stable blood sugar and blood pressure, strong cardiorespiratory fitness, and preserved muscle strength. It also includes consistent, restorative sleep; a well-regulated circadian rhythm; and resilience in the face of stress—meaning the ability to recover and adapt effectively.
These markers not only signify healthy mitochondrial function but also actively support and reinforce it over time.
Q. What’s the connection between mitochondria and longevity? If someone wants to invest in their mitochondrial health now for better aging later, where should they start?
Mitochondrial dysfunction has long been recognized as one of the hallmarks of aging. Recent work even suggests it may be central to the entire aging process, because mitochondrial impairment can help explain and connect the other pillars of aging—from genomic instability and telomere attrition to inflammation and cellular senescence. Processes like mitochondrial biogenesis, mitophagy, and dynamic remodeling are essential for maintaining cellular vitality.
When these systems falter, damaged mitochondria accumulate, fueling chronic inflammation (“inflammaging”) and organ decline. Interventions that enhance mitochondrial turnover and efficiency are increasingly being studied as strategies to extend both lifespan and healthspan.
From my perspective as a psychiatrist, this biology is especially relevant. People with mental illnesses are known to age prematurely and die far earlier than the general population. A recent meta-analysis found that individuals with mental disorders lose nearly 15 years of life, on average. My hope is that by integrating mitochondrial health into mental health care, we can help close this mortality gap—supporting not only longer lives, but healthier and more fulfilling ones.
Q. Are there certain biomarkers you track over time that give the clearest picture of mitochondrial health or improvement?
For tracking mitochondrial and metabolic health over time, I focus on a core panel of accessible biomarkers. During periods of active treatment changes, I monitor these every 3–6 months, and then annually: fasting insulin and glucose to calculate HOMA-IR, HbA1c, lipid ratios such as triglyceride-to-HDL, hs-CRP as a marker of inflammation, liver enzymes like ALT and GGT for metabolic stress, uric acid, vitamin D, B12 with methylmalonic acid, and iron indices.
Together, these offer a window into insulin sensitivity, inflammatory tone, and nutrient status—all closely tied to mitochondrial function. I also track fitness-related measures, such as grip strength and resting heart rate, since these functional outputs provide a real-world readout of mitochondrial capacity and resilience.
In reality, biomarkers of mitochondrial function remain a complex and evolving area of research. Biotech companies and mitochondrial scientists are actively working to develop more precise biomarker panels that can reliably measure mitochondrial health, but most of these tools are still in development and not yet available for routine clinical use.
Q. Are there any emerging therapies or protocols you’re most excited about for repairing or optimizing mitochondria?
Some of the most exciting emerging therapies for repairing and optimizing mitochondrial
function are coming from both lifestyle-based and targeted biologic approaches. One that I am especially enthusiastic about is ketogenic metabolic therapy, which our group has highlighted as a transdiagnostic intervention in psychiatry. Growing human data—including case series and pilot trials in people with serious mental illness—show meaningful improvements in both psychiatric symptoms and metabolic health, suggesting broad potential across diagnoses.
Other promising interventions include photobiomodulation with red and near-infrared light, which early randomized controlled trials suggest can reduce depressive symptoms by directly stimulating mitochondrial cytochrome-c oxidase. Creatine augmentation has shown signals of faster and larger antidepressant response, likely through supporting mitochondrial phosphocreatine shuttling. Similarly, acetyl-L-carnitine has meta-analytic evidence for reducing depressive symptoms and is notable because low circulating levels have been identified as a potential biomarker of major depression.
Together, these approaches reflect a new generation of interventions aimed at directly enhancing mitochondrial health as a pathway to better mental and physical health outcomes.
Join Us IRL
Start with your mitochondria. Then join us for another proven way to elevate energy levels: real, live, in person community.
Thousands will gather in West Palm Beach for Eudēmonia Summit, November 13–16.
Everything just hits different when you’re in the room.
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

February 20, 2026

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026