For much of the 20th century, psychedelics were treated as a threat to society. Today, they're being welcomed as treatment for it. Compounds once considered fringe and counterculture are now at the center of clinical research, medical use, and policy reform.
But this isn't entirely new territory. In spiritual circles, these medicines have always been respected for their ability to dissolve rigid thinking, surface buried truths, and reconnect individuals to something larger than themselves. What began in jungles and underground ceremonies is now showing up in peer-reviewed journals and FDA breakthrough designations.
The renaissance is unfolding across multiple fronts. Clinical studies reveal therapeutic benefits for depression, PTSD, and addiction that often surpass conventional treatments. Neuroimaging labs are mapping how these compounds rewire neural networks and restore brain plasticity. Policy reform is creating legal pathways for therapeutic access. And as research advances, we're moving from one-size-fits-all protocols toward personalized medicine—where genetics guide dosing, therapy meets neurochemistry, and healing is tailored to individual biology.
Yet describing psychedelic experiences remains like describing color to someone who's never seen light. No matter what is written about them, there is no substitute for direct experience. And decades of stigma—along with potentially challenging situations—have made people cautious. Rightfully so.
These substances demand courage and respect, and can be disorienting, physically uncomfortable, emotionally intense. They're not gentle medicines or quick fixes. But for many, navigating that difficulty becomes the catalyst for lasting transformation: clarity where there was confusion, connection where there was isolation, hope where there was despair.
Not everyone needs that journey. And there are real risks, real limitations, and real reasons to proceed with care. The field faces legitimate challenges around study design, safety protocols, and translating clinical results to real-world outcomes.
But the mounting evidence suggests we're witnessing something significant—a fundamental shift in how we understand consciousness, mental health, and human potential. Below, we move through the major psychedelic compounds gaining traction, tracing where the science stands and where it may lead.
The Four Frontiers of Psychedelic Healing
Mental Health Disorders
Psychedelics and empathogens are showing remarkable promise for some of the most stubborn psychiatric conditions. From treatment-resistant depression to PTSD, clinical trials have repeatedly demonstrated rapid and durable improvements—often after just 1–3 guided sessions. Patients report not only symptom relief, but also a renewed sense of perspective, agency, and emotional connection.
Unlike conventional treatments that often require daily medication, these compounds offer a more profound and punctuated model of healing—one that rewires rather than suppresses.
Addiction & Substance Use
Substance use disorders are notoriously difficult to treat, but psychedelics may offer a breakthrough. Rather than replacing one dependency with another, they appear to interrupt the underlying psychological and neurological patterns that drive compulsive behavior. Patients frequently describe confronting the root causes of their addiction—often trauma, isolation, or shame—in a setting that allows for emotional resolution and meaning-making. Long-term remission rates in early studies are outperforming many conventional approaches, especially when paired with skilled therapy and integration.
Brain Health & Cognitive Resilience
Beyond treating mental illness, a new frontier is opening around brain health. Psychedelics appear to enhance neuroplasticity, stimulate the growth of new synaptic connections, and reduce inflammation in ways that may support long-term cognitive vitality. Early research suggests potential applications in emotional regulation, learning, creative thinking, and even aging. While still early, this line of inquiry positions these compounds not just as medicine for what’s broken—but as tools to strengthen what’s already working.
Spiritual Health & Existential Well-Being
Not everything that needs healing is diagnosable. For many, psychedelics provide a path to meaning, perspective, and a deeper relationship with life. These substances have long been used in spiritual traditions to facilitate ego dissolution, mystical experience, and a sense of unity—with nature, with others, or with the divine. Today, those same effects are being explored in settings as diverse as hospice care and grief support. At their best, these experiences don’t just reduce suffering; they reconnect us to what makes life worth living.
Sponsor Message from Journey Clinical
The future of psychedelic therapy isn’t just about compounds—it’s about infrastructure, safety, and access.
Journey Clinical is leading that future. Their collaborative model empowers licensed psychotherapists to offer Ketamine-Assisted Psychotherapy (KAP) in private practice, supported by an in-house medical team for screening, monitoring, and prescribing with psychiatric medication management.
This keeps care anchored in the therapist–client relationship, while ensuring clinical oversight. And it works: 87% of patients report improvement in symptoms after a course of treatment.
Journey Clinical has also partnered with COMPASS Pathways to help shape how psilocybin-assisted psychotherapy can be delivered if approved by the FDA, from therapist training to real-world protocols.
In a field driven by potential, they’re focused on what makes it real: clinical rigor, accessibility, and systems that scale.
The compounds may lead the headlines—but Journey Clinical is building the care delivery system.
Microdosing: The Subtle Revolution
While high-dose psychedelics make headlines for their dramatic therapeutic breakthroughs, a quieter movement is reshaping everyday life. Microdosing—the practice of taking sub-perceptual amounts of compounds like psilocybin or LSD—has become a popular entry point for those seeking enhanced focus, emotional balance, and creative flow without the intensity of a full psychedelic experience.
The approach typically involves taking one-tenth to one-twentieth of a recreational dose every few days, often following systems like the Fadiman protocol (one day on, two days off) or the Stamets stack (psilocybin combined with lion’s mane and niacin). Anecdotal reports span the spectrum—from improved mood and cognitive flexibility to deeper empathy and subtle shifts in perspective that integrate seamlessly into daily routines.
Scientifically, the picture is more complex. Some studies suggest modest benefits for mood and neuroplasticity, while others argue the effects may be largely placebo. Measuring something meant to be sub-perceptual presents its own research challenges. But the cultural momentum is clear: from tech executives to burned-out parents, people are turning to microdosing as a gentle tool for mental and emotional resilience.
Its appeal lies not just in what it offers—but in what it doesn’t demand. No therapist, no ceremony, no surrender. It’s a path to optimization rather than transformation. Yet with that accessibility comes risk: less structure, more variability, and the potential for subtle dependencies masquerading as self-improvement.
Still, as science evolves and legal frameworks catch up, microdosing may emerge as a middle path—bridging the gap between underground experimentation and clinical use. A reminder that psychedelics don’t always need to be profound to be powerful.
A Compound-by-Compound Breakdown
Now, let’s take a closer look at the compounds themselves—what they are, what they’re doing, and where each one stands in this evolving field.
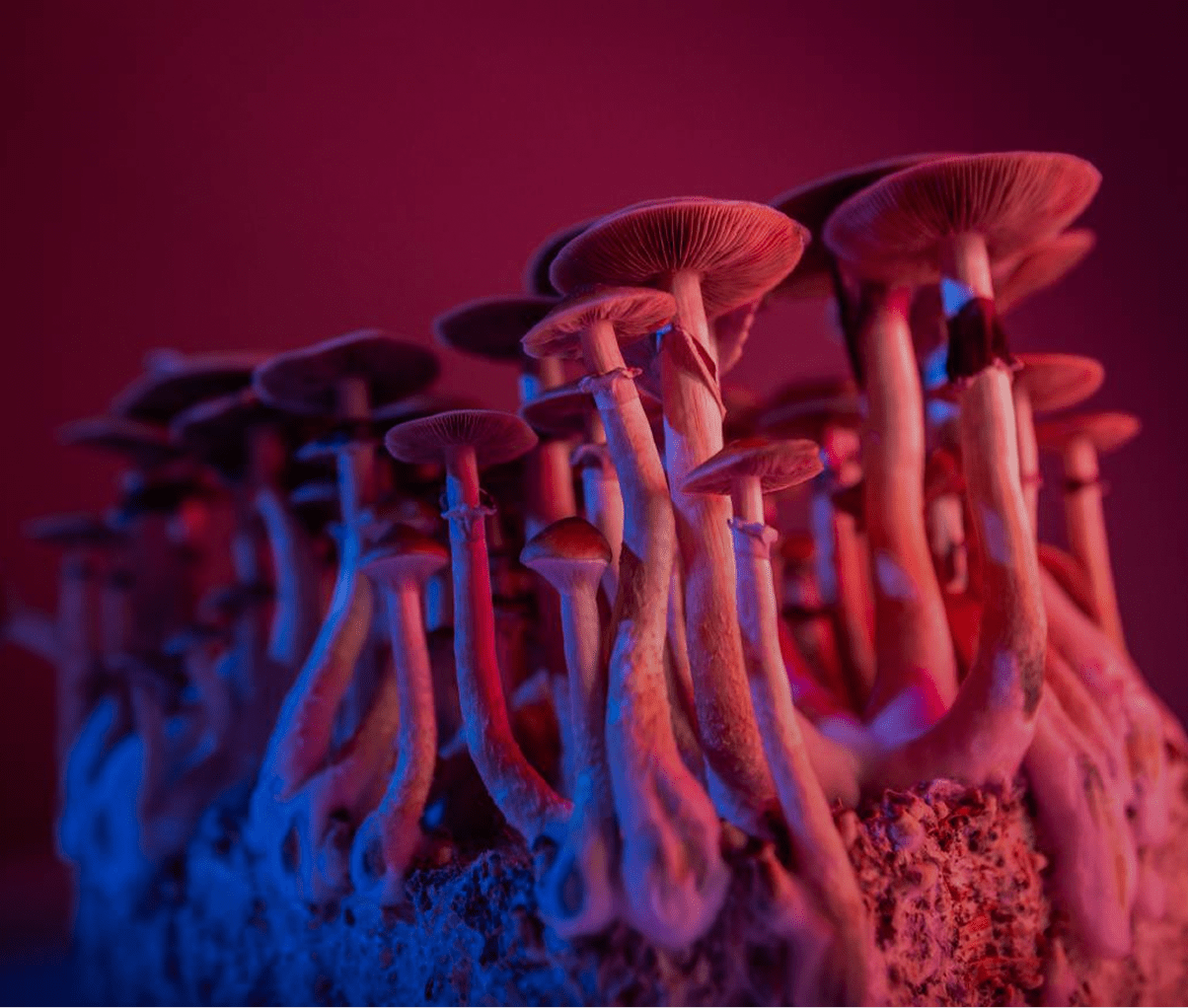
Psilocybin
Psilocybin is the active psychoactive compound found in over 200 species of “magic mushrooms.” When ingested, it converts to psilocin in the body, which acts primarily on serotonin 2A receptors in the brain.
Effects typically begin within 20–40 minutes and last 4–6 hours, producing altered visual perception, emotional amplification, and shifts in consciousness. Unlike synthetic drugs, psilocybin has been used by indigenous cultures for thousands of years and has a well-established safety profile with very low addiction potential.
Clinically, psilocybin is being studied—and in some cases, already used—to treat conditions like:
- Treatment-resistant depression
- End-of-life anxiety
- Obsessive-compulsive disorder
- Substance use disorders
But its benefits appear to reach further. Neuroimaging shows psilocybin increases connectivity between brain regions that don’t normally communicate, which may help “reset” entrenched patterns of thought and emotion—supporting both recovery and cognitive flexibility.
And for many, its impact is spiritual as much as neurological: the experience of ego dissolution, interconnectedness, or awe can leave lasting shifts in worldview, values, and meaning. Psilocybin, in other words, doesn’t just relieve suffering—it helps reorient the mind, the brain, and the self.
Regulatory Status
Psilocybin has received Breakthrough Therapy designation from the U.S. FDA for addressing treatment-resistant depression and major depressive disorder, helping to accelerate clinical research and development.
In 2023, Oregon became the first jurisdiction in the world to launch a legal psilocybin therapy program, allowing supervised adult use with trained, licensed facilitators. Colorado approved similar reforms, with a regulated therapeutic program expected to roll out in 2025. More than a dozen US cities—including Denver, Seattle, and Oakland—have decriminalized psilocybin, and several states are exploring therapeutic access or research programs.
Internationally, Canada permits limited therapeutic use of psilocybin under its Special Access Program for patients with serious or life-threatening conditions. In 2023, Australia reclassified psilocybin as a prescription-only medication for treatment-resistant depression, making it available through authorized psychiatrists in controlled medical settings.
More states and countries are likely to follow, as the evidence grows too compelling to ignore.
MDMA
MDMA (3,4-Methylenedioxymethamphetamine) is a synthetic compound that acts as both a stimulant and a mild psychedelic. It works by increasing the release of serotonin, dopamine, and norepinephrine, while also dampening activity in the amygdala—the brain’s fear center. Effects typically begin within 30–60 minutes and last 3–5 hours, producing heightened empathy, emotional openness, and reduced defensiveness.
Originally synthesized in the early 20th century, MDMA has demonstrated a favorable safety profile in clinical settings when administered with proper medical screening, psychological support, and therapeutic protocols. While not without risks, MDMA-assisted therapy for PTSD has shown promise in late-stage clinical trials under controlled conditions.
Clinically, MDMA is being studied—and is on the verge of approval—for treating:
- Post-traumatic stress disorder (PTSD)
- End-of-life anxiety
- Social anxiety in autistic adults
- Treatment-resistant depression (early stage research)
But MDMA’s value isn’t limited to clinical diagnoses. In therapeutic settings, it helps individuals access and process painful emotions without becoming overwhelmed—making it especially powerful for trauma work. Neuroimaging shows it increases connectivity between emotion and cognition networks while reducing fear responses, which may explain why difficult memories become more accessible, yet less distressing.
Spiritually and relationally, MDMA is often described as a heart-opening compound—one that fosters connection, compassion, and a felt sense of safety. Many report a renewed capacity for trust and intimacy, both with themselves and others. In that sense, MDMA doesn’t just heal trauma—it helps restore the conditions for human bonding and emotional wholeness.
Regulatory Status
MDMA received Breakthrough Therapy designation from the FDA for PTSD and showed promising results in two Phase III trials led by MAPS, with around two-thirds of participants no longer meeting PTSD criteria after three sessions. However, the FDA declined to approve MDMA-assisted therapy in 2024 due to concerns about study methods and safety, requesting further research.
In 2023, Australia became the first country to allow MDMA-assisted therapy under psychiatric supervision, and several US states are developing access frameworks in anticipation of future federal approval.
When approved, MDMA will be the first empathogen legally available for widespread clinical use—a major inflection point in the future of trauma treatment.
Ketamine
Ketamine is a dissociative anesthetic first synthesized in the 1960s and FDA-approved for surgical use in 1970. Unlike classic psychedelics, it works primarily by blocking NMDA receptors, which are involved in pain, mood regulation, and synaptic plasticity. At sub-anesthetic doses, ketamine produces a dreamlike, dissociative state that can include altered perception of time, space, and self.
Effects begin within minutes and typically last 45–90 minutes. Originally developed for human surgery and trauma care, ketamine also became widely used in veterinary medicine for its fast-acting, safe anesthetic properties. Today, it has quietly become one of the most widely available psychedelic therapies in the world.
Clinically, ketamine is already being used to treat:
- Treatment-resistant depression
- Suicidal ideation
- Generalized anxiety disorder
- Chronic pain syndromes
- PTSD (off-label use)
While not FDA-approved for PTSD, ketamine is widely used off-label in clinical settings, with growing evidence supporting its role in trauma relief and emotional reset.
But ketamine’s therapeutic value may go beyond symptom relief. Research shows it stimulates the rapid release of brain-derived neurotrophic factor (BDNF); promotes synaptogenesis; and enhances neuroplasticity, biological mechanisms that support healing, learning, and resilience.
Patients often describe the experience as emotionally clarifying—less a direct confrontation with trauma and more a spacious reframing of self and circumstance.
Though not traditionally associated with spiritual insight, some report profound states of ego detachment, inner stillness, or perspective shifts, especially when used with intention and integration support.
Regulatory Status
Ketamine is FDA-approved for anesthesia and for treatment-resistant depression. Spravato (esketamine) is available by prescription under strict clinical protocols, while generic ketamine is legally prescribed off-label for a wide range of conditions.
Dozens of ketamine clinics now operate across the US, offering IV, IM, nasal-spray, or lozenge-based treatments—though practices vary widely in quality and oversight.
Because it is already legal and prescribable, ketamine has become the most accessible psychedelic medicine in modern psychiatry—opening the door for a new model of rapid, non-daily treatment for mood disorders.
LSD
Lysergic acid diethylamide (LSD) is a semi-synthetic psychedelic that was first synthesized in 1938 by Swiss chemist Albert Hofmann at Sandoz Laboratories in Basel, Switzerland. It became widely known in the 1960s for its role in counterculture, but its roots lie in psychotherapy. Early practitioners explored its use for depression, alcoholism, and creativity.
LSD is one of the most potent psychedelics, active in microgram doses. It primarily affects serotonin 2A receptors, but it also influences dopamine and other neurotransmitter systems. Effects begin within 30–60 minutes and can last 8–12 hours, often producing vivid visual distortions, time dilation, deep introspection, and a sense of cosmic or existential awareness.
Clinically, LSD is being researched for:
- Anxiety associated with terminal illness
- Depression
- Alcohol use disorder
- Cluster headaches
- Emotional resilience and cognitive flexibility (early-stage research)
While it shares some similarities with psilocybin, LSD offers a longer and often more mentally intricate experience. Early studies suggest it may reduce rumination and improve mood in patients with anxiety or depressive symptoms. Some research also points to enhanced creative thinking and increased openness—a personality trait linked to psychological growth.
Spiritually, LSD has long been described as a consciousness-expanding substance. It can surface deep emotional material, evoke archetypal visions, and—at times—instill a profound sense of wonder, meaning, or interconnectedness. While not always comfortable, the depth of the experience has made it a tool for transformation in both clinical and ceremonial settings.
Regulatory Status
LSD remains a Schedule I substance in the US, with no current FDA breakthrough designations. However, research restrictions have eased in recent years. Clinical trials are ongoing in Switzerland, the US, and the UK, with organizations like MindMed and the Beckley Foundation leading studies into its therapeutic potential.
Compassionate use programs in Switzerland allow licensed therapists to work with LSD in controlled environments. No jurisdictions have legalized therapeutic use, but decriminalization measures in several US cities have included LSD in broader reforms.
As public perception shifts and research expands, LSD may soon re-enter the clinical landscape—not as a relic of the past, but as a precision tool for mental, cognitive, and existential health.
DMT & 5-MeO-DMT
DMT (N,N-Dimethyltryptamine) is a naturally occurring psychedelic compound found in hundreds of plant species—and in trace amounts in the human body. When inhaled or vaporized, it induces a powerful, immersive experience that lasts only 10–30 minutes but often feels much longer. Sometimes called “the God molecule,” DMT has long been associated with mystical experiences, encounters with otherworldly intelligence, and the dissolution of the self into something vast and ineffable.
5-MeO-DMT, a closely related compound found in certain toads (Bufo alvarius) and plants, produces a similarly intense but less visual experience often described as ego-erasing and profoundly unitive. Both are known for their rapid onset, overwhelming intensity, and deep spiritual or metaphysical content. Users frequently report a complete dissolution of ordinary reality, encounters with “other intelligences,” or the sensation of being reabsorbed into consciousness itself.
Clinically, these compounds are being investigated for:
- Treatment-resistant depression
- Anxiety and existential distress
- End-of-life preparation
- Addiction and compulsive behaviors (early trials)
Though research is still early, DMT and 5-MeO-DMT are showing potential as fast-acting antidepressants. In studies using intravenous DMT, people experienced quick improvements in mood—possibly because the drug makes brain activity more flexible and breaks the mental loops tied to depression and overthinking.
In therapeutic settings, these brief but profound experiences may allow patients to access deep emotional material, reframe existential fears, or shift ingrained psychological narratives.
Spiritually, these compounds are often described as life-changing—offering the kind of radical shift in perspective that people report after near-death experiences or moments of extreme clarity. 5-MeO-DMT, in particular, is known for inducing a complete loss of ego and a sense of oneness with all existence. When held in the right container, the result can be not only cathartic, but life-altering.
Regulatory Status
Both DMT and 5-MeO-DMT are Schedule I substances in the United States, making them illegal to manufacture, possess, or distribute. However, decriminalization measures in cities like Oakland, Santa Cruz, and Denver have removed local penalties for the use of plant-based DMT preparations. Colorado’s 2022 ballot initiative decriminalized natural DMT statewide, though synthetic forms remain prohibited.
Internationally, regulation varies. Some countries allow traditional use of DMT-containing plants (like ayahuasca), while synthetic DMT remains illegal. 5-MeO-DMT is less widely studied or regulated, though some retreat centers operate legally in Mexico and other jurisdictions.
As clinical trials expand and public interest grows, DMT and its analogs may soon shift from esoteric to essential in the evolving field of psychedelic medicine.
Ayahuasca
Ayahuasca is a psychoactive brew traditionally used in Amazonian healing ceremonies, made by combining two plants: Banisteriopsis caapi, which contains MAOI inhibitors, and Psychotria viridis, which contains the potent psychedelic DMT. On its own, DMT isn't active when taken by mouth, but the MAO inhibitors from the vine allow it to take effect when consumed as a tea, producing a 4–6 hour experience characterized by intense visuals, emotional (and physical) purging, and deep introspective insight.
Often referred to as a “plant teacher,” ayahuasca is not just a compound; it’s a cultural and spiritual practice. It is typically consumed in ceremonial settings, guided by experienced facilitators or shamans, and often accompanied by rituals, music, and integration practices.
Clinically, ayahuasca is being studied for:
- Treatment-resistant depression
- PTSD and trauma resolution
- Grief and loss
- Substance use disorders
Research suggests that ayahuasca may support emotional healing through a combination of psychological insight and neurobiological effects. It increases brain-derived neurotrophic factor (BDNF), modulates serotonin receptors, and may enhance mindfulness and emotional regulation long after the experience ends. Patients often describe encounters with symbolic or archetypal imagery, revisiting formative memories, or feeling reconnected to a deeper sense of purpose.
Spiritually, ayahuasca is revered for its capacity to confront the unconscious. Many report experiences that are not merely therapeutic, but transformational—catalyzing shifts in identity, relationships, and worldview. It is sometimes described less as a drug and more as an intelligence—something that shows, teaches, reveals.
Regulatory Status
Ayahuasca exists in a complex legal gray area. In the US, the Supreme Court has granted legal protection to specific religious groups to use ayahuasca in sacramental contexts. However, therapeutic use outside those contexts remains federally prohibited. Several US cities have decriminalized plant medicines, including ayahuasca, under local ordinances.
Internationally, countries like Peru and Brazil legally recognize and regulate traditional ayahuasca use, with retreat centers offering structured ceremonial experiences. However, safety, training, and ethical standards vary widely.
While formal medical access is limited, the growing body of research—and thousands of reported anecdotal outcomes—suggest that ayahuasca may soon play a larger role in integrative mental and spiritual health care.
Ibogaine
Ibogaine is a naturally occurring psychoactive extracted from the African shrub Tabernanthe iboga, traditionally used in Bwiti spiritual ceremonies in Gabon and Central West Africa. Unlike other psychedelics, it interacts with multiple neurotransmitter systems—serotonin, dopamine, NMDA, and opioid receptors—producing intense experiences lasting 12–24 hours. The journey typically unfolds in two phases: an initial flood of vivid, waking dream-like visions, followed by an extended period of deep mental processing and introspection.
Clinically, ibogaine is being used to treat:
- Opioid addiction and withdrawal
- Alcohol and stimulant dependence
- Trauma-driven compulsive behaviors
- Treatment-resistant depression (exploratory research)
What makes ibogaine unique is its potential to interrupt addiction at both the physiological and psychological level. Anecdotal reports and early studies suggest it can eliminate withdrawal symptoms, reset dopamine pathways, and reduce cravings after a single high-dose session. Patients often report reliving key emotional memories, processing long-buried trauma, and experiencing what some describe as a neurological “reset.”
Spiritually, ibogaine is considered a teacher rather than a tool—demanding, unfiltered, and unsparing. The experience is rarely euphoric but often life-altering. For many, it delivers hard truths and deep clarity—especially when paired with structured integration and support.
Regulatory Status
Ibogaine remains a Schedule I substance in the US, with no approved medical use. As a result, individuals seeking treatment often travel to clinics in Mexico, Costa Rica, New Zealand, and other countries where it is legal under medical supervision.
While clinical trials have been slow due to safety concerns, ibogaine’s track record in interrupting opioid dependency—at a time when overdose rates remain high—continues to draw interest from researchers, clinicians, and policy advocates alike.
Mescaline
Mescaline is a naturally occurring psychedelic found in several species of cacti, most notably peyote and San Pedro. Used ceremonially by Indigenous cultures across the Americas for thousands of years, mescaline produces an 8–12-hour experience often described as emotionally gentle, visually rich, and spiritually grounding. It works similarly to psilocybin and LSD, but with a distinctly different psycho-emotional character—often marked by clarity, empathy, and a heightened connection to nature and community.
Clinically, mescaline is being studied for:
- Depression and anxiety
- Alcohol use disorder
- Existential distress
- Emotional processing and personal growth
While formal research is limited compared to other psychedelics, early data and extensive ethnographic reports point to mescaline’s ability to facilitate emotional resolution, reduce fear and shame, and promote long-term shifts in perspective. Unlike faster-acting compounds, mescaline’s slower onset and extended duration give participants time to reflect, feel, and integrate as the experience unfolds.
Spiritually, mescaline is known for evoking reverence—for the earth, for life, and for one’s own place in the greater whole. It is less likely to induce ego dissolution than other psychedelics, but it often produces a strong sense of peace, clarity, and inner coherence. Many describe it as “clean,” “kind,” or “wise”—a companion for healing rather than a force to be reckoned with.
Regulatory Status
Mescaline remains a Schedule I substance under US federal law, but with a key exception. Members of the Native American Church are legally permitted to use peyote in religious ceremonies. San Pedro and other mescaline-containing cacti exist in legal gray zones—legal to own in many jurisdictions but illegal to consume.
Several cities have decriminalized mescaline-containing plants as part of broader plant medicine reforms, though synthetic mescaline remains prohibited. As the psychedelic field grows, mescaline may become more formally recognized not just as a therapeutic agent but a bridge between ancestral wisdom and modern emotional health.
The Promise and the Process
Despite the promising headlines and breakthrough designations, the psychedelic field faces significant challenges that deserve honest acknowledgment. Many studies suffer from small sample sizes, lack of proper blinding (it's hard to hide a psychedelic experience), and participants who are already believers in the treatment. The reproducibility crisis in psychology affects psychedelic research, too. Early enthusiasm doesn't always translate to sustained clinical benefits.
Side effects are also real, even if they’re less headline-friendly. Psychedelics often come with unpleasant physical effects like nausea, muscle tension, sweating, and a heavy body load that can last for hours. Psychedelics can provoke anxiety, panic, or dissociation. For individuals with a family or personal history of psychosis, they may carry serious risks. And while these compounds are not considered physically addictive, psychological dependence—or spiritual bypassing—can still occur.
The therapy component may be doing more heavy lifting than the drugs themselves, raising questions about whether expensive, controlled substances are necessary when intensive therapy alone might suffice. Additionally, the hype around psychedelics risks overselling benefits while underselling risks, potentially setting up patients and the field for disappointment.
But the evidence is still compelling—and growing.
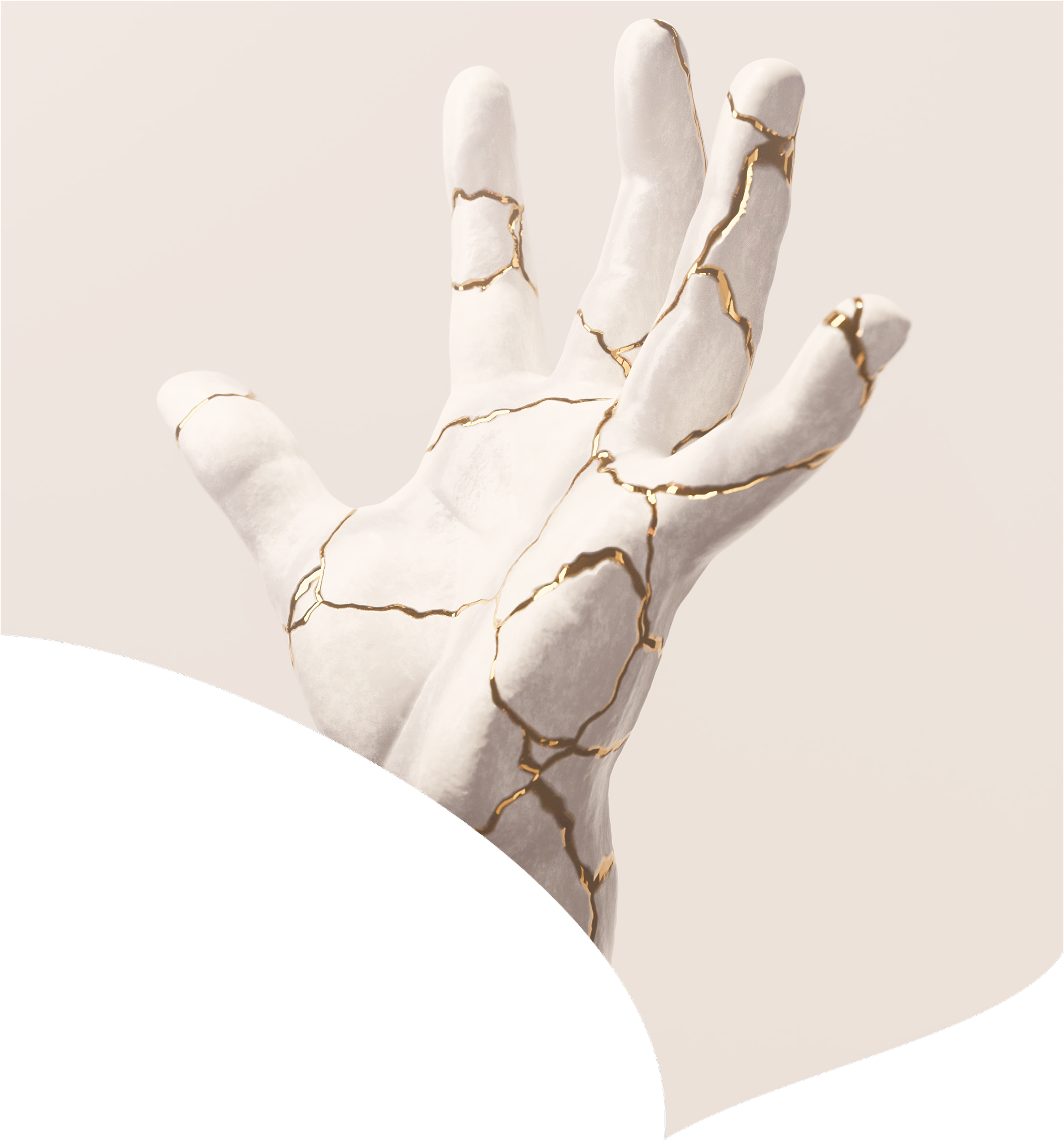
Psychedelics temporarily increase neuroplasticity—the brain’s ability to rewire itself. For a short window, the grooves of our thinking loosen. New patterns can form. Old ones can dissolve. It's a rare chance to reshape the architecture of the mind.
The challenge is not whether these compounds work, but how, for whom, and under what conditions. This is not a magic pill paradigm. If psychedelics are to fulfill their promise, they’ll need to be held with precision, patience, and humility. That means resisting hype in favor of rigor, and trading quick wins for sustainable breakthroughs.
The Future of Psychedelics
There are many other effective compounds (and stacks of compounds together) that will create states of mind and spirit we’ve barely touched—and that we’ll be hearing much more about in the years ahead. Some may be gentler, more targeted, or longer-lasting than the tools we know today. Others may challenge our assumptions about consciousness, healing, or even what it means to be human.
This movement is still taking shape. And it’s not for everyone. But if we meet it with curiosity, humility, and care, psychedelics may not just change how we heal. They may change how we live.
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

February 20, 2026

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026