Psilocybin is not new, but we are entering its renaissance.
It has been used ceremonially for centuries. Indigenous cultures understood it as spirit, teacher, or even portal. It vanished into the long shadow of prohibition, slipped underground and stayed there—stigmatized and misunderstood, then hardened into taboo during the anxious conformity of the 1950s. Then it reemerged through counterculture. And now it sits inside the walls of research labs and biotech start-ups and on the counters of CEOs and soccer moms.
Psilocybin has gone from underground ceremony to institutional review board. From sacrament to Schedule I to serious medicine.
In research hospitals, psilocybin is being studied for major depression and deep fear. In state legislatures, it’s being debated and decriminalized. In private clinics, guided sessions are being offered to people who feel stuck, depressed, burned out, or existentially untethered.
While many look to escape their reliance on pharmaceutical medication, psilocybin has become an increasingly popular alternative because of its power to radically alter perception, identity, and emotional processing.
But what exactly is this compound and what does it do to us?
Psilocybin and Rewiring the Brain
Psilocybin is a naturally occurring psychoactive compound found in over 200 species of mushrooms, primarily in the genus Psilocybe. Chemically, psilocybin is not active on its own. After you ingest it, your body quickly converts it into another compound called psilocin. Psilocin is the molecule that actually produces the psychological effects people associate with psychedelics.
Psilocin works because it looks a lot like serotonin, a chemical your brain already uses to regulate mood and perception. Because of that resemblance, it can attach to serotonin receptors, particularly one called 5-HT2A.
Those receptors play a central role in mood, perception, cognition, and the ongoing construction of the self.
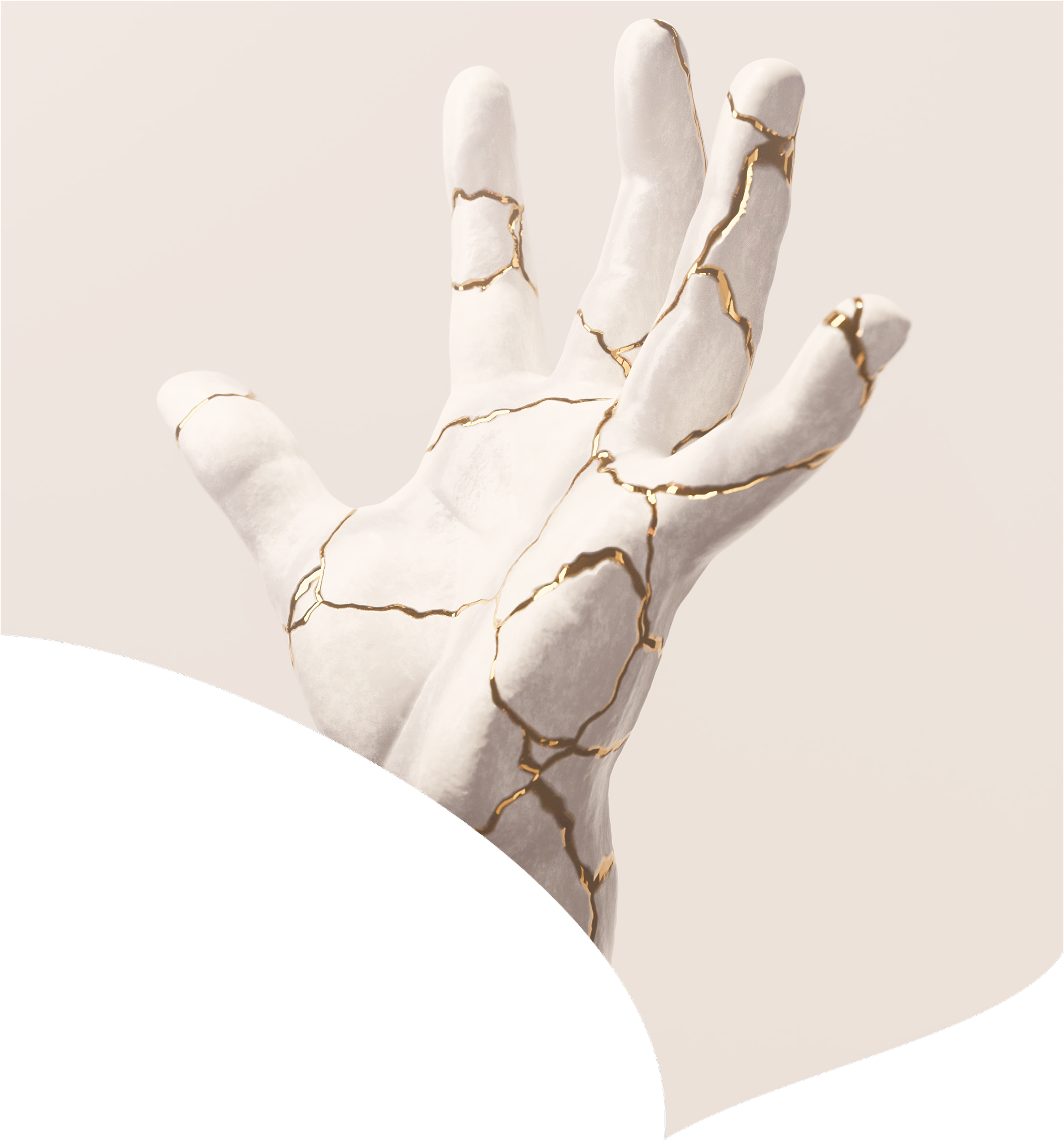
When psilocin activates the 5-HT2A receptor, the usual patterns of communication between brain regions begin to shift. Networks that typically operate in parallel start exchanging information more freely.The brain becomes less locked into its habitual pathways. Rigid loops soften and new patterns become possible.
A single dose can trigger measurable changes in neural connectivity and gene expression. In some studies, these shifts appear to persist long after the drug has cleared the body.
This stands in contrast to much of modern psychiatry over the past 60 years. Since the 1960s, treatment has largely centered on adjusting neurotransmitter levels day after day. Raising serotonin with SSRIs. Modulating dopamine with antipsychotics. Fine-tuning other chemical messengers in an effort to stabilize mood and behavior.
Underlying that model is a simple premise: mental illness reflects a chemical imbalance that requires ongoing management.
Psilocybin suggests a different model: that some psychiatric conditions might be better understood as “stuck” neural patterns—rigid networks that trap people in loops of rumination, anxiety, or compulsive behavior. Rather than daily symptom management or suppression, psilocybin appears to open a temporary window of heightened plasticity. During that window, patterns may loosen, making psychological change more possible. It’s less about correcting a chemical imbalance and more about interrupting the loop and resetting the system.
A Message from Our Partner
Mental health care is being rewritten, and it’s happening in Colorado.
The Wholeness Center in Fort Collins, Colorado, is the only licensed psilocybin-assisted therapy program in the country operating inside a full-service mental health clinic.
That distinction changes everything.
Most psychedelic therapy ends when the session ends. At Wholeness, it's just the beginning.
Preparation, facilitation, and integration are embedded within a true clinical ecosystem of licensed therapists, with ongoing support from a team that knows your history. This is real therapy with real continuity.
Healing from depression, trauma, or addiction isn't about one profound experience. It's about what happens in the days, weeks, and months that follow. Because real psychedelic therapy doesn't end when the session does—it deepens through follow-up, personalized treatment plans, and structured integration.
This is what responsible, effective psychedelic care looks like. And Wholeness is leading it.
To learn more about psilocybin therapy, the Wholeness method, and their amazing team, please visit their website.
Interrupting The Default Mode Network
Inside your brain is a network of regions that lights up when you are not focused on a task. When you’re daydreaming or your mind is wandering. Or when you’re thinking about the past or future.
Neuroscientists call it the Default Mode Network, or DMN.
It is deeply involved in autobiographical memory, self reflection, and what we experience as our sense of identity.
In depression, anxiety, and OCD, this network often becomes overactive and overly rigid. Brain imaging studies show excessive connectivity within the DMN and weaker communication with other networks. The result can feel like being trapped in repetitive loops of rumination, worry, or compulsive thought.
Psilocybin appears to interrupt that pattern.
In a 2024 study, researchers scanned participants’ brains repeatedly before, during, and after a single dose of psilocybin. They compared those changes to what happens after a dose of methylphenidate, a stimulant known as Ritalin.
Psilocybin produced substantially larger shifts in how brain regions communicated with each other. The most pronounced changes occurred in the Default Mode Network.
Rather than tightening networks, psilocybin seems to loosen them. Communication patterns become less rigid and the brain enters a more flexible state. That temporary flexibility may help create the conditions for longer lasting change. Researchers sometimes describe this as a “window of plasticity.” A period of heightened malleability during which entrenched patterns are easier to reshape.
Importantly, some of these changes persist for weeks after a single dose.
This may help explain why some people describe the experience as stepping outside their usual narrative about themselves. The network most associated with the “self” becomes quieter.
Neuroplasticity: Psilocybin Make Grow New Connections
Psilocybin does more than temporarily alter communication between brain networks. Emerging research suggests it may also promote structural change.
In animal studies, a single dose has been shown to trigger rapid growth of dendritic spines in the frontal cortex. These tiny protrusions are where synapses form. More spines mean more potential connection points between neurons.
In simple terms, the brain appears capable of building new wiring.
These effects appear to involve biological pathways long associated with learning and memory. When these systems are activated, they increase the production of proteins that strengthen synapses and help stabilize new connections between neurons.
In simple terms, the brain becomes more capable of reinforcing what it experiences.
More recently, researchers have begun to map how this rewiring unfolds. A 2025 study found that psilocybin’s effects on synapses are not random. The changes are activity dependent and network specific. Circuits that are active during the experience are more likely to be reshaped. Regions that are quiet tend to remain unchanged.
In simple terms, what the brain is doing during the experience appears to matter.
This may help explain why subjective experience correlates with therapeutic outcomes. The intensity of insight, emotional processing, or even mystical type experiences often predicts longer term benefit.
It is not that the drug alone heals. It is that psilocybin appears to create a biologically receptive state. A period of heightened plasticity during which active circuits can be remodeled.
The compound may open the window, but the experience, and what happens within it, may determine what changes.
Consciousness and Complexity
Under psilocybin, the brain does not quiet down. It becomes more dynamically organized. There is increased communication across networks that do not typically interact. Activity patterns grow less predictable, less confined to their usual routes.
Interestingly, this pattern is the opposite of what happens under anesthesia, where neural complexity collapses and consciousness fades. Psilocybin does not shut down the brain. It seems to open it up, allowing the emergence of novel thoughts, perspectives, and emotional states.
The Clinical Evidence
Psilocybin is rapidly emerging from the fringes of psychiatry into the center of serious clinical discussion, backed by a growing body of randomized trials. Below is a concise snapshot of some of the most compelling efficacy data to date.
Antidepressant Effects, Remission and Response Rates
antidepressant effects. A recent meta analysis pooling data from 436 participants found a large reduction in depressive symptoms compared to control conditions. By conventional statistical standards, the effect size was substantial, larger than what is typically observed in trials of standard antidepressants.
Beyond average symptom reduction, there is another way to look at the data from the meta analysis referenced above.
In these trials, participants who received psilocybin were roughly twice as likely to experience a meaningful clinical response, typically defined as at least a 50 percent reduction in depressive symptoms, compared to placebo or active placebo.
In other words, the effect is not just statistical. It translates into real people feeling substantially better.
In the same analysis, participants who received psilocybin were nearly three times as likely to fall below the diagnostic threshold for depression compared to control treatments.
That means not just feeling somewhat better, but no longer meeting criteria for major depression. It suggests that, in supported settings, psilocybin-assisted therapy may move a meaningful subset of people from “improved” to “in remission,” at least over the short to medium term. Long-term durability is still being studied.
Single Dose, Measurable Impact
In a randomized, double-blind trial of 104 adults with major depressive disorder, participants received a single 25 mg dose of psilocybin alongside structured psychological support.
At both 1 week and 6 weeks, the psilocybin group showed about a 12 point greater reduction on the Montgomery–Åsberg Depression Rating Scale compared to an active placebo. On that scale, a difference of that size is considered both statistically and clinically meaningful.
On average, people felt much less depressed—often moving down a whole category of severity—after one psilocybin session, compared with people who didn’t get it.
No serious treatment-related adverse events were reported in the trial, suggesting a favorable short-term safety profile when administered in a carefully controlled, supervised setting.
Durability
One of the most compelling questions is not whether psilocybin works in the short term, but whether the effects last.
In follow-up data from a psilocybin-assisted therapy trial for major depressive disorder, participants were assessed 12 months after treatment. A year after treatment, about 75 percent of participants were still at least 50 percent better than where they started.
And about 58 percent were doing so well that they no longer met the diagnostic criteria for depression. Participants were still meaningfully better than where they began, even 12 months after treatment.
There’s a 5-year study follow-up as well, where researchers found that about two-thirds remained in remission from depression, without ongoing medication or booster sessions. Participants described not just fewer symptoms, but a lasting shift in how they related to depression itself, experiencing it as more manageable rather than overwhelming.
It is important to note that these were relatively small samples and participants received structured psychological support before and after dosing. But the durability signal is difficult to dismiss.
For some individuals, a limited number of guided sessions appears capable of producing benefits that extend well beyond the acute experience.
Please note: The outcomes from above reflect guided sessions with screening, preparation, and follow up. Not unsupervised use. These are in clinics with licensed and trained medical professionals.
Integration is Important
In qualified clinical settings, there’s a process around therapeutic psilocybin. Psilocybin therapy typically involves preparation sessions, a supervised dosing experience lasting 4–6 hours, and structured integration afterward with a mental health professional. And the lasting therapeutic effect we mentioned above seems to arise from a combination of biological factors and psychological context.
Psilocybin can elicit anxiety, confusion, or painful memories. It can be a very uncomfortable or challenging experience. But in many cases, working through that discomfort is part of what makes the experience therapeutic.
That is where integration matters. Integration does not happen during the peak of the psychedelic experience. In that phase, participants are usually encouraged to turn inward, often lying down with eyeshades and music, supported quietly by trained therapists or facilitators who ensure safety and steadiness.
The interpretive work begins after the acute effects subside. Sometimes later that day. Often the following day. And then again in structured sessions over the weeks that follow.
In those conversations, therapists help participants process what emerged, translate insights, and integrate the experience into daily life.
Without that relational support, the effects become less durable.
This is why modern research protocols emphasize preparation and follow-up. Participants typically meet with therapists beforehand to establish trust and clarify intentions. They are supported during the dosing session. And they return for structured conversations afterward.
The Safety Profile
Psilocybin’s physiological safety profile in controlled settings is well-established. Cardiovascular effects are generally mild and transient. There’s no evidence of addiction potential or organ toxicity, and serious medical complications are rare.
But it is not risk‑free and is absolutely not a casual wellness product. Think “medication plus intensive psychotherapy in a monitored environment,” not “take a mushroom at home.”
There are common short-term side effects shortly after dosing and during the experience, and they include:
- Psychological: acute anxiety or panic, confusion, transient paranoia, emotional lability, and challenging or frightening experiences; these are common but usually manageable with skilled therapists and resolve as the drug wears off.
- Physical: nausea, vomiting, transient increases in heart rate and blood pressure, headache, dizziness, and fatigue over the following 24–48 hours
One major psilocybin trial in treatment‑resistant depression reported a small number of suicidal and self‑injurious events in the weeks after dosing, prompting important safety concerns, but pooled data across randomized trials so far suggest a modest overall reduction in suicidal ideation and no clear evidence of increased suicide attempts or deaths.
Certain populations face elevated risks. Individuals with personal or family history of psychotic disorders or bipolar disorder are typically excluded from trials due to concerns about triggering manic or psychotic episodes. Those with unresolved trauma may be particularly vulnerable to destabilizing experiences during sessions.
Larger, longer‑term studies are still needed to fully clarify risk.
States with Supervised Psilocybin Services
These states have or are implementing regulated frameworks for facilitated psilocybin “service” or “therapy” sessions in licensed settings (access generally does not require a specific diagnosis, but sessions must be supervised).
- Oregon: First statewide regulated psilocybin services program (Measure 109), with licensed facilitators and service centers operating since 2023.
- Colorado: “Natural medicine” framework (Proposition 122) with state‑regulated psilocybin services; personal use and home cultivation are decriminalized, but commercial retail sale is still prohibited outside the licensed system.
- New Mexico: Medical psilocybin access pathway created by recent legislation; rules are being finalized and full program implementation is planned for late 2026.
- Washington (state): Limited, research‑based psilocybin therapy pilot program run through a public university; access is primarily via approved research or pilot sites.
Where Do We Go From Here?
We are entering a pivotal moment.
One pharmaceutical‑grade psilocybin formulation (Compass Pathways’ COMP360) is already in Phase 3 trials for treatment‑resistant depression, while others are advancing through late‑stage development.
Usona is testing a high‑purity psilocybin formulation for major depressive disorder, and Cybin’s deuterated analog CYB003 has received FDA breakthrough therapy designation after encouraging Phase 2 remission and response rates.
The science is maturing and the regulatory process is underway. But there are other challenges ahead before this becomes more widely available. Current protocols are resource intensive and expensive. They require trained therapists, dedicated treatment environments, and significant clinician time for each session. If these medicines are approved, millions of Americans could theoretically qualify. That raises urgent questions about training, cost, infrastructure, and equitable access.
Some researchers are exploring whether compounds can be designed to promote neuroplasticity without producing the full hallucinogenic experience. In theory, that could increase scalability, but it remains an open question whether removing the subjective experience eliminates a crucial therapeutic component.
The research and data is piling up. The anecdotal evidence is impossible to dismiss. Psychedelic medicine is emerging as a real tool, helping some people step off the hamster wheel of traditional pharmacological treatment and into periods of meaningful psychological change.
Is it for everyone? Is it a magic bullet? No, of course not. But it’s clear that it works for many, and it might work for you or your loved ones.
I’m grateful to be living at a moment when we are beginning to address the roots of suffering, not just its symptoms, and to have tools that aim to restore health rather than simply manage decline.
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026

January 2, 2026