We’re witnessing a pharmaceutical phenomenon unlike any other in modern medicine.
Few other classes of drugs in modern medical history have achieved this combination of adoption rate, sales velocity, and cross-demographic impact.
In less than a decade, a class of injectable peptides moved from diabetes clinics into dinner conversations, celebrity interviews, and supermarket aisles. They’ve challenged our assumptions about metabolism, redefined the idea of willpower, and forced medicine to confront a new question: What if metabolism can be rewired?
The Scale of the GLP-1 Boom
These are the most famous weight-loss drugs ever created—and maybe the most effective. GLP-1s have reshaped global healthcare economics and the business models of food companies, and created a social phenomenon.
- 1 in 8 American adults has tried a GLP-1 drug, and half are still taking one
- As of September 2024, they account for 5% of all prescriptions in the U.S.
- Sales of Ozempic and Wegovy are outpacing Apple’s revenue growth rate
- Novo Nordisk’s (the company behind Ozempic and Wegovy) market cap briefly surpassed Denmark’s GDP
- Novo Nordisk reports that at least 25,000 people in the US are starting Wegovy each week—five times more than in December 2023
- The appetite-suppressant market they created could hit $144 billion by 2030
But what exactly are these drugs? Where did they come from? And perhaps most importantly, what do we really know about their long-term effects?
We're not here to advocate for or against these medications. We're here to present the full picture: the remarkable benefits, the significant risks, the economic realities, and the many unknowns that make this one of the most complex medical decisions of our time.
What Are GLP-1s and Where Did They Come From?
GLP-1 stands for glucagon-like peptide-1, a naturally occurring hormone released from the gut after we eat. Its job is to tell the brain and pancreas that food has arrived, which slows digestion, stimulates insulin, and signals fullness. In other words, GLP-1 helps control blood sugar and appetite.
The first synthetic GLP-1 analog was approved in 2005 to help people with type 2 diabetes manage blood sugar, but an unexpected side effect—reduced appetite and weight loss—hinted at something much larger.
Nearly two decades of refinement later, that side effect became the main event. Modern formulations like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) mimic the body’s natural GLP-1 signal more potently and last far longer than earlier versions, fundamentally reshaping how millions of people experience hunger and satiety.
What began as a glucose-control therapy has evolved into a powerful metabolic intervention, one that may eventually redefine how medicine approaches obesity, aging, and energy balance.
The Current Landscape
Today’s GLP-1 market is dominated by several key players:
- Semaglutide: Marketed as Ozempic for diabetes, Wegovy for weight loss, and Rybelsus (oral form)
- Tirzepatide: Sold as Mounjaro for diabetes and Zepbound for weight loss
- Liraglutide: Available as Victoza for diabetes and Saxenda for weight loss
- Dulaglutide: Known as Trulicity for diabetes
North America dominates with 64% of the global GLP-1 market share as of 2024. Among users, more than 60% take them for managing chronic conditions like diabetes or heart disease, while about 40% use them solely for weight loss.
How GLP-1s Work
Think of GLP-1 drugs as a master switch that affects multiple systems in your body,
- Your stomach empties slower. Food stays in your stomach longer, keeping you full.
- Your brain gets stronger “I'm satisfied” signals. The constant food chatter so many people live with finally quiets.
- Your body releases insulin more efficiently. Better blood sugar control comes without the spikes.
- Your appetite naturally decreases. You simply want to eat less.
The result is fast, often dramatic reductions in body weight, driven by both biology and behavior working in sync. But these mechanical changes tell only part of the story. The deeper effects go beyond appetite. GLP-1s shift how the body uses and stores energy, improving insulin sensitivity, slowing digestion, and reducing food cravings and the drive to eat for pleasure rather than hunger.
What once required constant willpower starts to feel more manageable, as biology begins working with you rather than against you.
The Benefits (Beyond Weight Loss)
The effects extend far beyond what the scale says:
Cardiovascular Protection
The FDA approved Wegovy as a cardiovascular medicine after studies showed it could reduce heart attacks and strokes in overweight people. The reduction in overall mortality risk (19%) has caught the attention of longevity researchers.
Potential Addiction Treatment
Anecdotal reports of reduced cravings for alcohol and other substances are being investigated by companies like Eli Lilly.
Alzheimer's Prevention
Research examining records of a million people found that taking semaglutide was associated with a 40% to 70% lower chance of an Alzheimer's diagnosis. Large international studies are now underway to confirm these findings.
Sleep Apnea
In December 2024, the FDA approved tirzepatide (Zepbound) for treating moderate-to-severe obstructive sleep apnea in adults with obesity.
Kidney Protection
In January 2025, semaglutide (Ozempic) received FDA approval to reduce the risk of kidney disease worsening in adults with type 2 diabetes and chronic kidney disease.
The Concerns and Criticisms
While the benefits are exciting, the enthusiasm surrounding GLP-1s must be tempered. These are powerful drugs with risks, unknowns, and limitations that anyone considering them needs to understand.
The Side Effects Are Real and Can Be Severe
About half of users experience nausea, and one-third deal with diarrhea. But the gastrointestinal issues go deeper. Some report persistent vomiting, severe constipation, and gastroparesis—a condition where the stomach essentially stops working properly. The gastroparesis risk is 3.7 times higher than with other weight-loss medications, and while it affects less than 1% of users, it can be debilitating and potentially permanent.
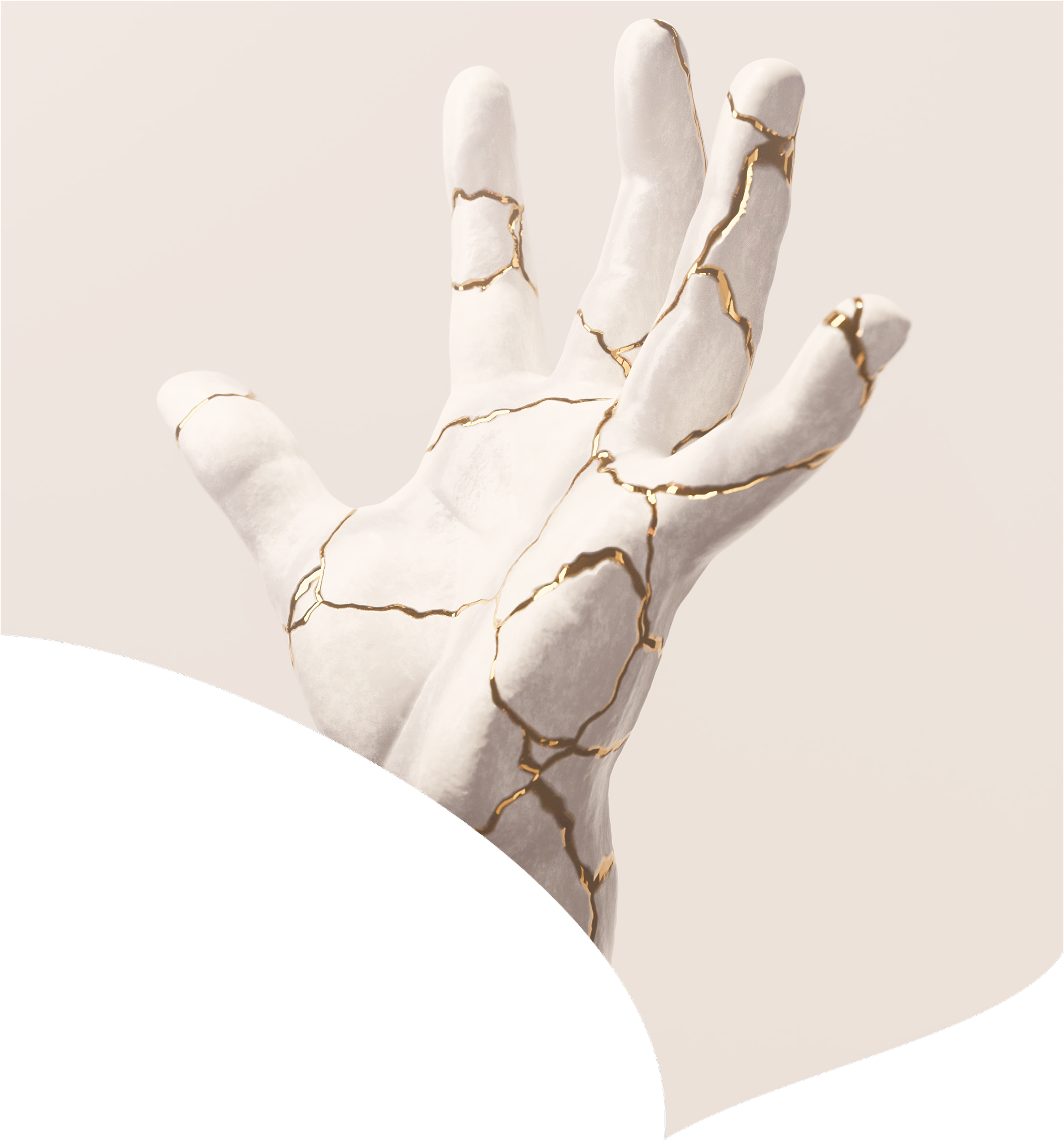
The Weight Loss Isn’t Just Fat
Up to 40% of the weight lost comes from muscle mass, not fat. This means people may end up smaller but metabolically worse off, with reduced strength and bone density. The rapid weight loss can also cause “Ozempic face”—a gaunt, aged appearance from facial volume loss.
Most People Regain The Weight
Between 50–75% of users stop within a year due to side effects, cost, or other factors. When they do, clinical data shows they regain about two-thirds of their lost weight within twelve months. For many, this becomes an expensive, temporary intervention rather than a lasting solution.
We Don't Know the Long-Term Consequences
These drugs have only been widely used for weight loss for a few years. What happens after a decade or two of use? What about interactions with aging, other medications, or life changes like pregnancy? We're conducting a massive real-world experiment with limited long-term data.
The Long-Term Question
The “lifetime drug” debate is perhaps the most challenging aspect. Since patients regain weight after stopping, and the medications’ long-term safety beyond a few years remains unknown, users face a difficult decision.
The Financial Cost is Staggering
At over $1,000 per month, GLP-1s have created a healthcare divide based on wealth. Only 24% of insured users get full coverage while 19% pay entirely out of pocket, often spending $12,000+ annually. Medicare can't legally cover weight-loss prescriptions, and explosive demand has created shortages that leave diabetics unable to access medications they need for blood sugar control as supply goes to weight-loss patients willing to pay premium prices.
The Psychological Questions
While appetite suppression can feel liberating, some users report feeling disconnected from food entirely, losing the ability to enjoy meals or eating socially. Others worry about psychological dependency. What happens to your relationship with food and eating when a drug is managing your hunger signals?
The reality is that for all their promise, GLP-1s remain imperfect tools with significant trade-offs that many users discover only after starting treatment.
The Future of Weight Loss Drugs
Here's what most people don't realize: the GLP-1 revolution we're witnessing now is actually just the opening act. The pharmaceutical industry has identified metabolism as the next great frontier, and the pipeline of drugs in development is staggering.
We're not just talking about incremental improvements; we're looking at treatments that could fundamentally reshape how medicine approaches weight, aging, and metabolic health.
Triple Agonists
While most people are still figuring out Ozempic, Eli Lilly's retatrutide is preparing to make current drugs look outdated.
Triple agonists attack the problem from three different angles simultaneously:
- GLP-1 pathway: suppresses appetite (like current drugs)
- GIP pathway: improves how your body processes the food you do eat—better insulin response, improved fat metabolism
- Glucagon pathway: actively increases energy expenditure and fat burning, essentially turning your metabolism up (this is the game-changer)
In trials, people are losing 24-30% of their body weight, numbers that rival gastric bypass surgery. We're talking about a 300-pound person dropping to 210 pounds with injections alone. FDA approval could come as early as 2026, and if it does, it could make today's “miracle drugs” obsolete by comparison.
But retatrutide isn't alone. Pfizer, Amgen, and several biotech companies have their own triple agonists in development, each with slightly different mechanisms and potentially different side effect profiles. The race is on to create the most effective, tolerable version.
Oral Versions and Other Delivery Mechanisms
Weekly injections have been the biggest barrier to widespread adoption. They require medical oversight, proper storage, and create a constant reminder that you're “on medication.” The industry recognizes this, and the solutions coming will transform how people access these treatments.
Novo Nordisk's oral semaglutide for weight loss should receive FDA approval by late 2025, but it’s just the first wave. There are currently 63 oral GLP-1 drugs in development, with four in Phase III trials.
But the innovation goes far beyond pills. The next generation of delivery systems will make treatment nearly invisible:
- Transdermal patches that deliver steady doses through the skin, eliminating both injections and the need to remember weekly doses. It’s still early and experimental, as getting peptides through the skin remains a challenge.
- Quarterly implants that dissolve slowly under the skin. Imagine getting a tiny implant every three months instead of weekly injections. This could be revolutionary for compliance and access in underserved areas.
- Nasal sprays for rapid-acting appetite control before meals, allowing people to target specific eating situations rather than maintaining constant medication levels.
The Next-Generation of Metabolic Drugs
The industry is moving beyond hormone mimetics to target metabolism at the cellular level.
Companies are developing:
- Leptin sensitizers that help your brain properly recognize the “I’m full” signals that many overweight people have become resistant to
- Brown fat activators that literally turn your body into a more efficient calorie-burning machine
- Mitochondrial enhancers that improve how your cells produce and use energy
- Gut microbiome modulators delivered as engineered probiotics that reshape your metabolic environment from the inside out
Many of these are in clinical trials right now.
The Markets and Regulatory Landscape
The first GLP-1 patents start expiring in 2026–2027. When generic competition hits, prices could drop 8–-90%. Meanwhile, biosimilar manufacturers in India and Eastern Europe are preparing to flood the market with affordable versions.
But the real game-changer might be manufacturing innovation. Companies are developing new production methods that could bring costs down to $50–100 per month instead of $1,000+. At those prices, insurance coverage becomes a non-issue, and global access becomes realistic.
The FDA is already signaling major changes in how they evaluate metabolic drugs. They're considering approving drugs for “metabolic health” rather than just specific conditions, potentially opening the door for broader use. Some experts predict that by 2030, taking a metabolic optimizer could be as common as taking a daily vitamin.
Where Do We Go From Here?
GLP-1s represent both tremendous promise and some justified uncertainty. They're not miracle drugs, nor are they dangerous medications to be feared. They're powerful tools that, like all medical interventions, come with trade-offs.
What’s clear is that they are here to stay. The pharmaceutical pipeline is packed with more effective, more convenient, and eventually more affordable options. Within a decade, taking a metabolic optimizer could be as routine as taking a statin or blood pressure medication.
Yet the current reality remains complex. With 50–75% of users discontinuing within a year due various factors, these drugs clearly aren’t the right solution for everyone. The decision to use them should be made with full knowledge of both benefits and risks, in consultation with healthcare providers who understand your individual medical picture.
What’s undeniable is that these drugs have permanently changed the conversation around obesity, metabolism, and modern medicine’s role in shaping behavior. Whether that change leads to progress, dependence, or something in between is still unfolding, and it will depend on how thoughtfully we navigate the choices ahead.
The metabolic revolution is just beginning. The question isn't whether these drugs are perfect—they're not. The question is how we'll use them wisely.
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026

January 2, 2026