Last Saturday, we explored the rise of GLP-1 medications—Ozempic, Wegovy, Zepbound—and what they reveal about how the human body actually regulates weight, hunger, and metabolic health. These drugs are transforming not just medicine, but culture itself.
Missed it? You can catch up on The GLP-1 and Weight Loss Revolution Issue.
We learned that GLP-1s aren’t shortcuts; they’re signals. They reveal what happens when biology and behavior fall out of sync—and how we might bring them back into balance.
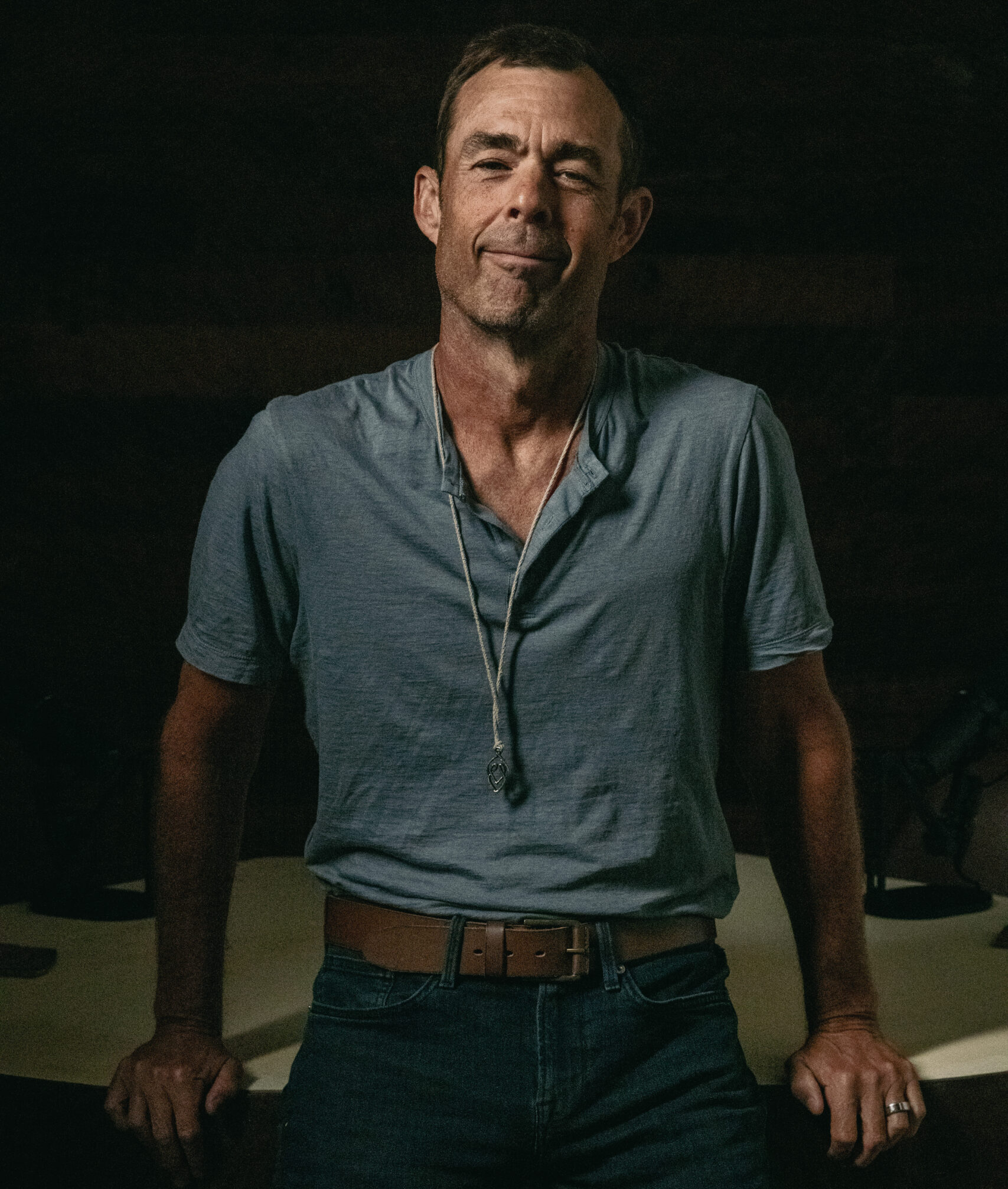
To help us understand the path forward, we turn to Ashley Koff, RD, for a grounded look at what metabolic health really means in the age of GLP-1s.
Ashley is an award-winning personalized nutrition expert. Koff’s a triple threat as a practitioner, consultant and speaker, helping thousands get and stay healthy powered by better nutrition. Today, as the founder of The Better Nutrition Program, Koff leads a team developing cutting-edge personalized nutrition tools and programs to optimize health.
With over 25 years of experience, Ashley has turned the idea of “better choices” into practical tools that empower individuals and healthcare professionals to achieve lasting health outcomes. She's been recognized as Hollywood’s Leading Nutritionist (InStyle) and one of CNN’s Top 100 Health Makers. She’s also the author of Recipes for IBS and Mom Energy, and her third book, Your Best Shot, debuts January 2026.
Q. It feels like everyone’s taking Ozempic now, even people who look perfectly healthy. Is there any other real reason to go on it if you’re not struggling with your weight?
Looking “perfectly healthy” does not mean that the body is operating healthfully. The first step in a weight-health approach (versus the longstanding approach of a weight or health focus) is moving on from total weight as an effective marker of anything. “Weight health” means your body’s weight composition—fat, muscle, bone and water—reflect the body’s operational health. We can’t know this with only total weight or appearance.
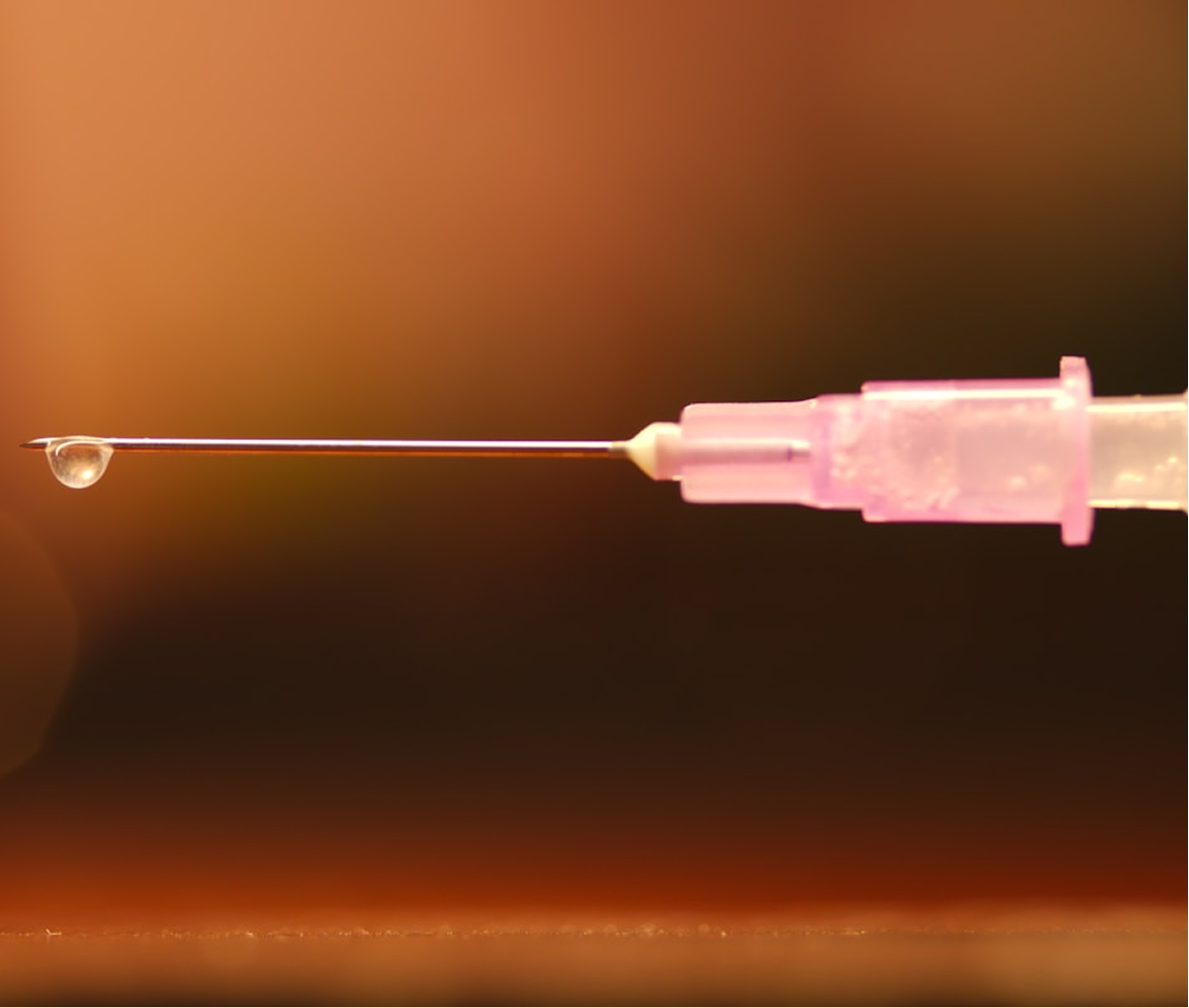
Our weight-health hormones (GLP-1, GIP, PYY, CCK) regulate weight health—our levels of fat, muscle, bone, blood sugar, appetite, hydration, and more. Their suboptimal function translates to impaired weight health. Regardless of appearance, a person may use a weight-health hormone replacement like semaglutide or tirzepatide (the ingredients in the branded medications like Ozempic, Zepbound, Wegovy) as a tool to help them optimize their weight health.
These medications are a biosimilar form of our own internal weight-health hormones. The key difference is that instead of staying active for 2–5 minutes, the medications (by design) last 24x7 and therefore lead to a dramatic increase and sustained hormone levels at the receptor sites throughout the body.
In addition to treating excess fat loss, these medications are approved for sleep apnea and diabetes. Many people also choose to use them to quiet “food noise” that contributes to disordered eating, to help prevent diabetes by improving blood sugar control in pre-diabetics, to reduce visceral fat in the liver even when overall body fat is within a healthy range, and to lower unhealthy levels of inflammation.
The medication is a tool, not a solution. We all need properly functioning weight-health hormones, and that’s achievable with a personalized plan—whether or not you use a GLP-1 medication.
For anyone using the medication, this is essential. While it offers benefits, it can also disrupt weight-health hormone balance—issues that often existed beforehand, which is why the medication was needed in the first place. Therefore, both short- and long-term success depend on optimizing internal weight-health hormone function.
Q. What are the real risks of GLP-1s? And are there certain people who should avoid them at all costs?
Speaking of cost, the ability to sustain the cost of the medication and the practitioner to provide ongoing assessment and optimization of a personalized plan is a huge risk factor, as insurance often doesn’t cover one or both. As someone treating hundreds of patients on these medications, let’s unpack other risks.
You have to stay on them forever. I don’t have a crystal ball about anyone’s life or health so I can’t say for sure one way or not. But I can share that if you use the medication and it has benefits, but your weight-health ecosystem worsens (muscle loss, metabolic slowdown, nutrient depletion, digestion worsens etc.), then you won’t be able to come off of them without weight regain. They are a hormone replacement. They likely suppress your own hormone production, especially at higher doses. I use a plan to wean and monitor, then a maintenance dose, then experiment with being off the medication if that works for the patient.
They cause you to lose muscle . . . or hair. Don’t blame the medication; they don’t directly cause muscle or hair loss. When that happens, it’s usually the result of a non-personalized or incomplete nutrition and lifestyle plan. For example, a person might be told to eat more protein, but if their digestion isn’t allowing them to properly absorb and use it, muscle and hair loss can occur. The same is true when nutrient imbalances are present, either because they existed beforehand or developed while on the medication. And if strength training and recovery aren’t well-matched to that person’s needs, the body won’t be able to build or maintain muscle or bone.
They increase risk of . . . several conditions, from ocular stroke to thyroid cancer to “frozen stomachs.” There are alarming headlines about these, but they need more context. For example, while a smaller ocular nerve could raise the risk of certain strokes, that’s true regardless of medication use. Likewise, though thyroid cancer has appeared in some studies, clinicians I follow have not seen this in patients taking Ozempic or similar drugs. The same goes for digestive problems. Since these medications slow stomach emptying, people already using proton pump inhibitors (PPIs) or other digestive aids may need a more personalized plan to prevent worsening symptoms. My overall advice is to work closely with your practitioner to assess personal risk and build a plan to reduce it—through lower doses, regular screenings, and ongoing monitoring of digestion, body composition, and nutrient levels.
Q. Do people who stop taking Ozempic tend to gain back the weight they’ve lost? Shouldn’t there be some responsibility from those prescribing it to educate their patients on better lifestyles?
Regaining weight is likely unless there’s a plan to recalibrate how the body’s own weight-health hormones function once the medication is stopped. The same thing happens when you stop a statin, a proton pump inhibitor, or almost any medication without first addressing the root cause of why you needed it. I believe the responsibility is shared—among the patient, the practitioner, the media, and the companies selling the medication or GLP-1 optimizer supplements.
As a patient, take responsibility and make sure whoever prescribes the medication helps you assess and create a plan to maintain your results. If your financial or health situation is changing and you know you’ll need to stop the medication, reach out early to avoid stopping suddenly without a weaning or maintenance plan.
If you’re with a company that sells these medications and you rely on AI evaluations or practitioners who don’t have the time—or the incentive—to provide thorough, ongoing assessments, you must clearly tell customers that they’ll need this support elsewhere.
If you’re with a supplement company or not a licensed medical practitioner, it’s essential to stay within ethical and legal boundaries. Marketing should never blur the line into medical education or recommendations that could mislead people into thinking your products will work the same way as prescription medications.
Q. How long can people stay on GLP-1s like Ozempic and WeGovy? Can they be on these drugs forever? Can we assume any long-term risks?
Again, I don’t have a crystal ball. But we do have some key insights about this class of medication.
They are biosimilar, not bioidentical. This means the drugs mimic—but aren’t identical to—our natural hormones. As a result, they change how the body functions both immediately and over time. These shifts are what create the benefits, but they can also introduce challenges to the body’s overall ecosystem.
Anecdotally, I see many patients whose fatigue coincides with a decline in heart rate variability while taking the medication. This fatigue is often attributed to eating too little, but mechanistically, the drug keeps the body metabolically “switched on” rather than in a true “rest and digest” state. While undereating can certainly cause fatigue, this effect can as well; over time, it may become a risk factor if not properly managed.
Are there other side effects that signal someone should stop the medication? Perhaps. But in the patients I’m seeing, the opposite is often true—they’re recalibrating their lives and choices in ways that improve both mental and physical health. Many are coming off other medications, healing their relationship with food, and finding peace with past traumas and “diet INFObesity.”
Q: I started taking Zepbound for mild weight gain after menopause and noticed something unexpected—my sleep apnea improved almost immediately, even before I’d lost much weight. Most of what I’ve read says the benefit comes from weight loss. But in my case, it seems to be doing something more. Do GLP-1 drugs have any direct effect on sleep apnea beyond reducing body fat? And if so, would that mean continuing on a low dose might help keep it under control long-term?
Since you’re not already my patient, I have a lot of questions. Yep, that’s the way this works!
We need to know about your current digestive and cardiometabolic history and how you sleep (open mouth, mouth versus nose breathing, flat or on your side or elevated)? How is your oral health, including the size of your tongue compared to your mouth? When did you eat your last meal and what did it contain? Do you drink alcohol? What is your stress like throughout the day?
The list goes on.
How does this relate to sleep apnea? Long seen as a condition caused by excess fat around the neck or upper body that shifts upward when lying down, sleep apnea is now understood as a disorder of the broader weight-health ecosystem. It’s not just about physical weight but about how hormones, metabolism, and inflammation interact to affect the body’s ability to regulate breathing, energy, and recovery during sleep.
And we know that GLP-1 is one of several weight-health hormones that regulate how your body functions, including how it will function during sleep (its “recovery window”). Yes, there is an obstructive component. But there is also a muscular and metabolic component.
By helping to promote better insulin (and glucagon) response, GLP-1 in your body or as a hormone replacement medication will improve your sleep and your sleep apnea. If you’re on a GLP-1 medication, and you are able to optimize your upper body muscle function and reduce the brain overactivity of food noise and improve your breathing while awake and asleep, it will help you resolve sleep apnea.
The key point for me is that evidence showing GLP-1 medications can help resolve sleep apnea shouldn’t mean that everyone with sleep apnea needs a prescription. Instead, it should prompt a major shift in how we assess, prevent, and treat sleep apnea—with personalized plans tailored to each person, whether they use a GLP-1 medication or not.
We’re at a true inflection point, largely because of the development of this class of medication. The current GLP-1 agonists are powerful tools for some people (I’m not referring here to the next generation of nonpeptide small-molecule GLP-1s), but their greater value lies in what they’ve revealed—how the human body really operates, the essential role of weight-health hormones, and the importance of keeping them functioning optimally for everyone.
If we apply these insights to create better assessments, personalized plans, and updated recommendations, we have a chance to course-correct as a society and build lasting, generational weight health. That’s awesome, right?

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026

January 2, 2026