Glucose is the body’s primary fuel. Every thought, movement, and heartbeat depends on it. But the way we regulate that fuel shapes far more than most people realize.
For decades, glucose has been treated as a “diabetes problem.” If your fasting numbers didn’t raise alarms at a yearly checkup, the assumption was simple: you’re fine. But research is now showing that blood sugar stability is central to how we feel and how we age, whether or not we ever receive a diagnosis.
Energy crashes in the afternoon, brain fog after lunch, restless sleep, stubborn weight gain, and accelerated inflammation all trace back to how the body handles glucose. It’s not just about preventing disease. It’s about everyday performance, long-term resilience, and longevity itself.
The truth is straightforward: blood sugar is not a niche metric. It’s a universal signal of health.
And yet, even among experts, the angles differ. Some argue sugar itself is the culprit. Others point to insulin resistance driven more by dietary fat than glucose. Some say to eat your carbs around exercise. Add in the distinctions between natural sugars in fruit, complex carbs, and refined processed foods, and the picture gets more complicated.
The stakes are high, because glucose touches everything:
- How sharp your mind feels in the moment,
- How well your body repairs at night,
- How much energy you can bring to the people and work you care about, and
- How long you’ll stay healthy as the years stack up.
Understanding blood sugar isn’t just about numbers on a lab test, it’s about the rhythms of your daily life and the trajectory of your healthspan.
In this issue, we’ll look closely at what the evidence actually says, and look for consensus among the experts. But we won’t be covering diabetes. That’s a big topic and for another issue.
The Basics: What Glucose Is & How It Works
Glucose is a simple sugar, but it’s the cornerstone of metabolism. When you eat carbohydrates—whether bread, rice, fruit, or vegetables—your body breaks them down into glucose. It’s important to note that the body can also produce glucose internally when dietary sources are low. That glucose enters the bloodstream, where it becomes the primary energy source for your muscles, organs—and especially your brain, which consumes about 20% of the body’s glucose at rest.
To keep glucose at safe, usable levels, the body relies on insulin. Insulin is a hormone made in the pancreas that acts like a key: it unlocks cells so they can take in glucose and use it for fuel. Without insulin, or when cells stop responding well to it, blood sugar rises. Too little glucose and you can’t think clearly or move with strength. Too much, and over time it damages tissues, accelerates aging, and raises the risk of chronic disease.
Most people only hear about glucose when doctors talk about diabetes, but the reality is that all of us ride a blood sugar curve every day. Spikes after meals, dips between them, and the body’s continual adjustments shape how stable our energy and mood feel. It’s this everyday rhythm, not just extreme highs or lows, that makes glucose worth paying attention to.
The Consequences of Dysregulation
When blood sugar runs too high, too low, or swings wildly throughout the day, the effects ripple across nearly every system in the body. Some consequences are immediate and easy to feel. Others are subtle, accumulating damage for years before they finally show up as chronic disease.
Short-term effects:
- Energy crashes and fatigue
- Intense cravings and hunger swings
- Mood volatility and irritability
- Brain fog and reduced focus
- Restless sleep and disrupted recovery
Long-term effects:
- Metabolic dysfunction: insulin resistance, prediabetes, and types 1 and 2 diabetes
- Cardiovascular disease: higher risk of heart attack, stroke, and hypertension
- Fatty liver disease: accumulation of fat in the liver, often silent until advanced
- Obesity and weight gain: driven by hormonal imbalances and increased appetite
- Kidney damage: elevated glucose slowly impairs kidney function
- Nerve damage: neuropathy causing pain, tingling, or numbness
- Eye disease: higher risk of retinopathy and vision loss
- Cancer risk: elevated glucose and insulin can drive tumor growth in some contexts
- Cognitive decline: increased risk of dementia and Alzheimer’s, sometimes referred to as “type 3 diabetes”
- Accelerated aging: glucose instability drives oxidative stress, chronic inflammation, and cellular damage
Glucose dysregulation often develops quietly. You can have “normal” labs while repeated spikes and dips are already reshaping metabolism, eroding blood vessels, and impairing organs. By the time fasting glucose or HbA1c numbers rise into the danger zone, the damage is often years in progress.
Blood Sugar Ranges: Normal vs. Optimal
When doctors measure blood sugar, they’re usually looking for levels high enough to diagnose diabetes or low enough to cause immediate danger. But there’s a big difference between what’s considered “normal” for avoiding disease and what’s optimal for long-term health and performance.
Fasting Glucose (first thing in the morning, before eating):
- Normal: 70–99 mg/dL
- Pre-diabetes: 100–125 mg/dL
- Diabetes: 126 mg/dL or higher
- Optimal: many longevity researchers suggest 75–85 mg/dL as a healthier daily target, since higher levels within the “normal” range still correlate with greater risk over time.
Post-Meal Glucose (1–2 hours after eating):
- Normal: generally under 140 mg/dL
- Optimal: closer to under 120 mg/dL, with a relatively smooth return to baseline within a few hours.
Big spikes above 140, even if occasional, can contribute to inflammation and oxidative stress.
Hemoglobin A1c (HbA1c, a 3-month average of blood sugar)
- Normal: under 5.7%
- Pre-diabetes: 5.7–6.4%
- Diabetes: 6.5% or higher
- Optimal: often cited as 4.8–5.2% for people aiming at longevity and metabolic health.
“Normal” ranges are designed to flag disease, not necessarily to guide you toward peak health. Staying on the lower, steadier side of these ranges—without dipping into dangerous lows—is where most experts agree the body functions best.
Common Myths We Need To Address
Much about glucose and blood sugar remains misunderstood, and decades of confusion have fueled misinformation. Let’s debunk some of it here.
Myth: There are universal “good” and “bad” foods for blood sugar
We all have individual metabolic fingerprints. . One of the most surprising lessons from modern glucose research is how differently people respond to the same food. For decades, nutrition advice was built on population averages: eat more of this, avoid too much of that. But continuous glucose monitoring and large-scale studies have revealed there’s no single “normal” response.
The landmark 2015 Weizmann Institute study followed 800 adults, continuously monitoring their blood sugar over a week while tracking diet, activity, sleep, and microbiome composition. The results were striking: the same food could cause sharp spikes in one person and almost no rise in another. In some cases, “healthy” foods like tomatoes or bananas produced unexpected glucose surges, while bread had minimal impact in others. The study concluded that individualized nutrition, guided by data, was far more accurate than universal dietary rules.
Subsequent research has confirmed this variability. A 2020 study in Nature Medicine examined over 1,000 participants in the UK and US and found wide differences in glucose and insulin responses, even among identical twins. The gut microbiome emerged as a powerful driver of these variations, reinforcing the idea that each of us has a unique metabolic fingerprint.
It isn’t just the food itself that matters. Sleep quality, stress levels, muscle mass, exercise timing, and circadian rhythms all influence how glucose is handled. Oatmeal can spike one person into a pre-diabetic range while keeping another stable. Eggs and avocado may be steady fuel for some, but not for others.
The takeaway is clear: there are no universally “good” or “bad” foods when it comes to blood sugar. Instead, each of us carries a unique signature, a personal fingerprint that determines how we process the same meal.
Myth: “Fruit is basically candy.”
While fruit contains fructose, it comes packaged with fiber, water, and nutrients that slow absorption. An apple creates a completely different metabolic response than a candy bar with equivalent sugar content. The dose, delivery method, and context matter enormously.
Fiber creates physical barriers. The fiber in fruit forms a gel-like matrix in your digestive tract that physically slows sugar absorption. It's like the difference between drinking sugar water through a straw versus through a sponge. The sugar has to work its way through this fibrous network, creating a gradual release rather than a flood.
Water dilutes the sugar concentration. An apple is about 85% water, which means the sugar is already diluted when it hits your system. Candy is concentrated sugar with minimal water content, creating a much higher sugar density that overwhelms your absorption mechanisms.
Cellular structure requires work. In whole fruit, the sugars are locked inside plant cells. Your digestive system has to break down these cell walls to access the sugar, which takes time and energy. Candy has already done this work for you—the sugar is immediately bioavailable.
Fructose vs. glucose ratios matter. Fruit contains both fructose and glucose, but in different ratios than processed sweets. Fructose is primarily processed by the liver and doesn't spike blood glucose as dramatically as pure glucose or sucrose.
Nutrients influence absorption. Fruit contains compounds like polyphenols and organic acids that can slow sugar absorption and improve insulin sensitivity. These create a metabolic context that processed sugar lacks.
Volume and satiety are important factors. You'll feel full after eating two apples (about 50g total sugar), but you can easily consume 50g of sugar in candy without feeling satisfied, leading to continued eating and higher total sugar intake.
This is why the "delivery system" matters as much as the sugar content itself.
Myth: “Carbs at night make you fat.”
Your metabolism doesn’t shut down at a certain time each evening. Recent research suggests eating carbs in the evening can actually improve sleep quality and next-day insulin sensitivity for many people. Total calories and overall patterns matter more than meal timing.
Serotonin and melatonin production improves when you eat carbs, which increase tryptophan uptake in the brain. Tryptophan converts to serotonin and then melatonin, improving sleep quality. Better sleep directly improves next-day insulin sensitivity, while poor sleep makes you temporarily insulin resistant.
Cortisol regulation benefits from evening carbs, which help lower cortisol levels. High cortisol from stress or circadian disruption raises blood glucose and promotes fat storage, especially around the midsection. Evening carbs can help normalize this stress hormone pattern.
Growth hormone optimization occurs during deep sleep, when your body releases growth hormone that helps with fat burning and muscle recovery. Stable blood sugar from evening carbs can improve sleep quality and enhance this natural growth hormone release.
Muscle glycogen timing works in your favor if you exercise earlier. After training, your muscles are more insulin sensitive and ready to soak up glucose to replenish glycogen stores. That means evening carbs are more likely to be directed toward recovery and repair rather than stored as fat.
Circadian insulin sensitivity naturally decreases slightly in the evening, but this isn't necessarily bad. It's part of your natural circadian rhythm, preparing your body for the overnight fasting period. Fighting this rhythm can be more disruptive than working with it.
Psychological factors play a role, because restricting carbs at night often leads to late-night cravings and poor food choices. Allowing moderate evening carbs can prevent the restrict–binge cycle that actually does lead to weight gain.
The key is that your metabolism operates on 24-hour cycles, not arbitrary cutoff times.
But important to restate the above: total calories matter more than when you eat your carbs.
The Science Is Evolving
Researchers are uncovering surprising ways that everyday habits, hormones, and even your microbiome shape how your body manages blood sugar.
Your gut bacteria influence your blood sugar.
New research reveals that your gut microbiome significantly influences glucose response. The trillions of bacteria in your digestive system don't just break down food, they actively shape how your body processes glucose and produces metabolic signals.
Two people can eat identical meals and see completely different blood sugar patterns based on their gut bacteria composition. This explains why personalized nutrition approaches are becoming more sophisticated than generic dietary advice. Your bacteria literally have a say in your metabolic destiny.
The “dawn phenomenon” isn't just for diabetics.
Many healthy people experience a natural rise in blood glucose upon waking, driven by cortisol and growth hormone. This morning glucose surge was historically seen as a red flag, something that only happened in people with metabolic dysfunction.
But it's actually a normal part of circadian metabolism that prepares your body for the day ahead. Your body is essentially starting its metabolic engine, releasing stored glucose to fuel your brain and muscles as you transition from the fasted state of sleep to active wakefulness.
Exercise timing creates metabolic advantages.
Exercising within 30 minutes after eating can reduce glucose spikes by up to 30%. Your muscles become glucose-hungry after meals, ready to pull sugar from your bloodstream for immediate fuel rather than letting it circulate and potentially cause problems.
But here's the surprising part: even light activity like a 10-minute walk is remarkably effective. You don't need to hit the gym or break a sweat. Simply avoiding prolonged sitting after meals allows your muscles to act as natural glucose sponges.
Cold exposure has an impact on glucose regulation.
Cold therapy appears to improve insulin sensitivity and glucose uptake. When your body is exposed to cold, it activates brown fat—a special type of fat tissue that burns glucose and regular fat to generate heat.
Regular cold exposure through cold showers, ice baths, or even just spending time in cooler temperatures can enhance this process. While research is still emerging, the metabolic benefits extend beyond just glucose control to include improved fat burning and stress resilience.
The CGM Revolution
Continuous glucose monitors (CGMs) are transforming our understanding of metabolism. These small sensors, worn on your arm like a patch, measure glucose in your tissue fluid every minute, 24 hours a day. What started as a medical device for diabetics is becoming the fitness tracker for metabolism.
Unlike traditional blood tests that capture a single moment, CGMs reveal the full movie of your glucose patterns. They show how your morning coffee affects your focus at 10:00 a.m., why you crash after lunch, and whether that evening snack disrupts your sleep. For the first time, we can see cause and effect in real time.
The data is often surprising. Many discover that their “healthy” smoothie creates a glucose roller coaster, while foods they avoided might barely register. Some find that stress from a difficult meeting spikes their glucose more than dessert. Others learn that a brief walk after dinner prevents the glucose rise they never knew was happening.
This isn't about achieving perfect numbers; it's about understanding your unique patterns. CGMs reveal which foods give you sustained energy versus quick crashes, how sleep quality affects next-day glucose stability, and why certain times of day feel naturally more energetic. The insights are deeply personal and often counterintuitive.
As CGM technology improves and costs decrease, they're likely to become as common as fitness trackers. Future versions will integrate with other health metrics—heart rate, stress markers, sleep patterns—to create a complete picture of metabolic health.
This real-time feedback could revolutionize preventive medicine. Instead of waiting for annual blood work to reveal problems, we'll spot metabolic drift years earlier. CGMs might become the early warning system that helps millions avoid diabetes, optimize athletic performance, and understand the daily rhythms that support peak cognitive function.
Managing Your Glucose Response
In addition to the basics, like avoiding processed and junk foods, and maintaining regular resistance and cardio training regimens, there are other things you can do to manage your blood sugar.
Move After You Eat
Just 10–15 minutes of light activity—a brief walk, some stretching, or even standing while doing household tasks—can significantly blunt glucose spikes. The key is to avoid prolonged sitting. But regular exercise is a fundamental way to manage your blood sugar.
Protein and Fat as Glucose Moderators
Starting meals with protein or healthy fats slows glucose absorption. This doesn't mean avoiding carbs; it means eating them in context. A piece of cheese before your apple, nuts with your oatmeal, or olive oil on your bread all help create gentler blood sugar curves.
Hydration Matters
Being even mildly dehydrated concentrates your blood, making glucose spikes appear more severe. Drinking water before meals helps with proper dilution and can reduce the perceived intensity of blood sugar swings.
Manage Your Stress
Since stress hormones raise blood glucose, stress management becomes blood sugar management. Brief breathing exercises, cold water on your wrists, or stepping outside for fresh air can interrupt the stress-glucose cycle.
Sleep Is Important
Consistent sleep timing helps regulate the hormones that control glucose. Even if you can't sleep more, sleeping and waking at the same times helps maintain your circadian glucose patterns.
Fiber as Your Glucose Buffer
Fiber slows sugar absorption by creating a physical barrier in your digestive tract. Adding fiber-rich foods to meals—vegetables, beans, nuts, or even a tablespoon of ground flaxseed—can significantly reduce glucose spikes. The fiber doesn't have to come from the same food as the carbs; a side salad can moderate the impact of pasta just as effectively.
Intermittent Fasting and Time-Restricted Eating (TRE)
Intermittent fasting and TRE have been shown in multiple studies and meta-analyses to reduce fasting glucose levels, lower insulin resistance and decrease average insulin concentrations in people with metabolic syndrome or prediabetes.
The Longevity Connection
Glucose control isn’t just about avoiding diabetes. It’s emerging as one of the central levers for slowing biological aging. The reason is simple. Unstable blood sugar drives the same processes that wear down the body over decades: chronic inflammation, oxidative stress, and mitochondrial dysfunction.
Advanced Glycation End Products (AGEs)
Chronically elevated glucose accelerates the formation of AGEs—sticky molecules that bind to proteins, impair their function, and damage tissues. Research from the Joslin Diabetes Center and others has shown that AGEs contribute to vascular stiffness, kidney disease, and visible skin aging.
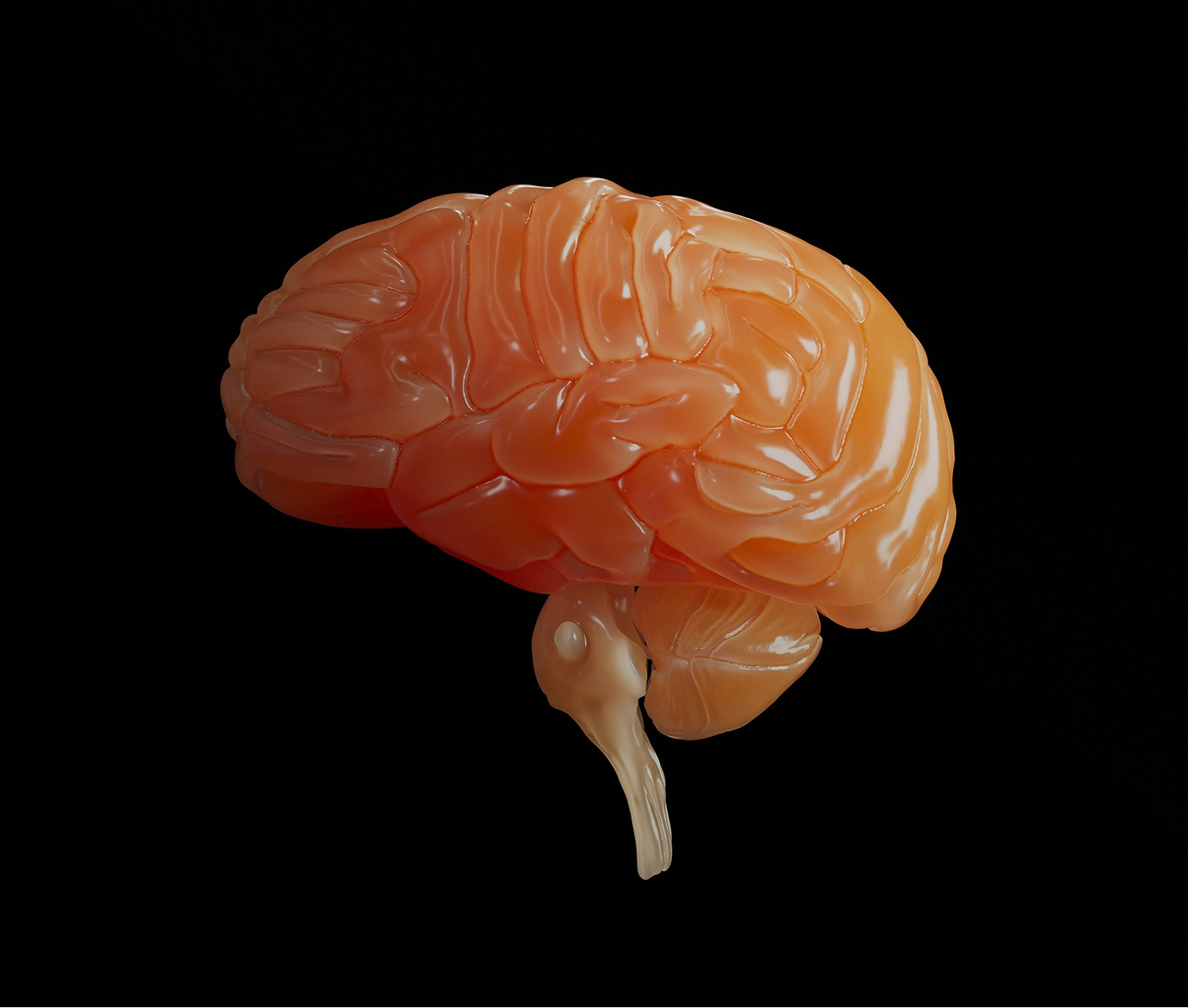
Brain Health
The link between glucose dysregulation and cognitive decline is striking. A 2013 study in The New England Journal of Medicine found that even modestly elevated fasting glucose, still below the diabetic threshold, was associated with a higher risk of dementia. Researchers now describe Alzheimer’s disease as “type 3 diabetes” because of its connection to impaired insulin signaling in the brain.
Mitochondrial Function
Excess glucose impairs mitochondrial efficiency, leading to reduced energy production and greater oxidative stress. Animal studies show that dietary and pharmacological strategies that stabilize glucose improve mitochondrial health and extend lifespan.
Stable glucose, on the other hand, supports mitochondrial efficiency, balanced hormones, and reduced systemic inflammation. In human longevity studies, blood sugar regulation consistently appears as one of the strongest predictors of extended healthspan.
For all the excitement around stem cells, gene editing, and advanced therapies, one truth remains clear: keeping glucose stable may be one of the most powerful, low-tech ways to slow aging.
The Future of Glucose Management
We're entering an era where glucose optimization will become as personalized as fingerprints. Within the next decade, continuous glucose monitors will likely shrink to the size of a contact lens or integrate directly into wearable devices. Real-time algorithms will learn your unique patterns and predict glucose responses before you eat, suggesting meal timing and composition based on your sleep, stress, and activity data.
Precision medicine is moving beyond one-size-fits-all approaches. Genetic testing combined with microbiome analysis will create detailed metabolic profiles that predict which foods, supplements, and lifestyle interventions work best for your biology. Instead of generic dietary advice, you'll receive recommendations calibrated to your specific genetic variants for glucose transport, insulin sensitivity, and circadian rhythm regulation.
The pharmaceutical landscape is expanding beyond diabetes management. Compounds like berberine and alpha-lipoic acid are being refined into targeted formulations, while GLP-1 receptor agonists originally designed for diabetes are showing promise for metabolic optimization in healthy populations. Smart drug delivery systems will release precise doses based on real-time glucose readings.
Perhaps most intriguingly, the boundaries between food and medicine are blurring. We're seeing the development of glucose-modulating probiotics, engineered foods with built-in glucose buffers, and even smart insulin patches that respond automatically to blood sugar changes. The goal isn't just managing diabetes; it's optimizing human performance through metabolic precision.
This future isn't decades away. Much of this technology exists in early forms today, waiting for refinement, regulation, and cost reduction to make it accessible to everyone seeking peak metabolic health.
The Bottom Line
Glucose management isn't about achieving perfect numbers or eliminating all spikes. It's about creating sustainable patterns that support steady energy, stable mood, and long-term health. The goal isn't metabolic perfection, it's metabolic flexibility and resilience.
Your relationship with blood sugar is deeply personal, influenced by genetics, lifestyle, stress levels, sleep quality, and dozens of other factors. What works for your friend might not work for you.
That's not a failure. It's biology.
The most powerful insight from recent glucose research isn't a new supplement or eating schedule. It's the understanding that small, consistent actions compound into significant metabolic improvements. A brief walk after dinner, protein with breakfast, awareness of your stress patterns . . . these simple changes can transform how stable and energized you feel throughout the day.
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

January 23, 2026

January 16, 2026
January 16, 2026

January 9, 2026

January 9, 2026

January 2, 2026

December 26, 2025
December 19, 2025