What if you could heal a torn ACL without surgery? Regrow heart tissue after a heart attack? Or one day, reset your entire immune system using your own cells?
Not in some distant future, but right now. In elite recovery centers, clinical trials, and high-end longevity clinics, stem cell therapy is being used to regenerate tissue, reduce inflammation, and intervene in diseases once considered untreatable.
Stem cells have been a medical curiosity for decades. But in the last few years, they’ve taken center stage. Today, these remarkable cells stand at the intersection of cutting-edge science, medical breakthrough, and controversial hype—potentially revolutionizing how we think about healing, aging, and treating disease.
Stem cells are often at the center of the story when a star athlete recovers from a career-threatening injury without surgery, when a patient with an "incurable" condition finds new hope, or when a longevity clinic offers rejuvenation at five-figure price tags. This isn't just medicine; it's the beginning of what many experts call the regenerative revolution—where treatments don't just mask symptoms but empower the body to heal itself.
That’s a key idea—and one we’ll return to again and again. Whether we’re talking about diet, supplements, peptides, or stem cells, the goal is always the same: to create the ideal conditions for the body to heal, recover, and restore itself.
The body has extraordinary intelligence.
In this deep dive, we break down:
- The types of stem cells and how they work
- Where they’re being used right now
- What delivery methods are actually effective
- Scientific breakthroughs on the horizon
- Risks to watch for
Regenerative medicine isn’t fringe anymore. Stem cell therapy is stepping into the mainstream—and with it, a new paradigm for how we think about healing, resilience, and human longevity.
HOW STEM CELLS WORK
Stem cells are the body’s raw materials—unspecialized cells with the unique ability to develop into many different cell types. But their true power lies in what they do, not just what they become.
When introduced into the body, stem cells do three things:
- Respond to biochemical distress signals. They migrate toward areas of injury or inflammation.
- Release signaling molecules. These signals (often via exosomes) instruct nearby cells to repair, regenerate, or calm immune activity.
- Transform when needed. In some cases, they can become the specific cell type needed—like cartilage, muscle, or nerve tissue.
It’s not just about replacement—it’s about communication. Stem cells act like conductors in the body’s healing orchestra, coordinating recovery and repair.
TYPES OF STEM CELLS
There are several different types of stem cells, each with their own origin, purpose, and promise.
Mesenchymal Stem Cells (MSCs)
These are the MVPs in many of today’s most promising therapies. MSCs are some of the most widely used stem cells in regenerative medicine today. They’re typically harvested from your bone marrow, body fat, or umbilical cord tissue. What makes them special is their anti-inflammatory and immune-calming properties. They're also excellent at helping the body repair itself. That’s why they’re being used for everything from arthritis and orthopedic injuries to autoimmune conditions and even age-related degeneration.
Hematopoietic Stem Cells (HSCs)
These cells live mostly in bone marrow, circulating blood, and umbilical cord blood. These are the cells responsible for creating all the different types of blood cells in your body. They’re already widely used in medicine today—especially in bone marrow transplants for people with blood cancers like leukemia and lymphoma, or genetic blood disorders like sickle cell anemia.
Pluripotent Stem Cells (iPSCs)
These are adult cells—often skin or blood cells—that scientists reprogram in the lab to act like embryonic stem cells. Because they can become almost any type of cell in the body, they hold incredible potential for personalized therapies. These show potential to do things like growing new heart tissue from your own cells. The science isn’t quite there yet, but the research is accelerating fast.
Perinatal Stem Cells
These stem cells are derived from birth-associated tissues such as the umbilical cord (including Wharton’s Jelly), placenta, and amniotic fluid and membrane. These are some of the youngest, most powerful stem cells, rich in healing and immune-supporting potential. They're still being studied, but early results are exciting—showing potential to accelerate tissue repair, calm autoimmune flares, and promote faster recovery in orthopedic injuries. Many parents now choose to bank their child’s cord blood as a potential future resource.
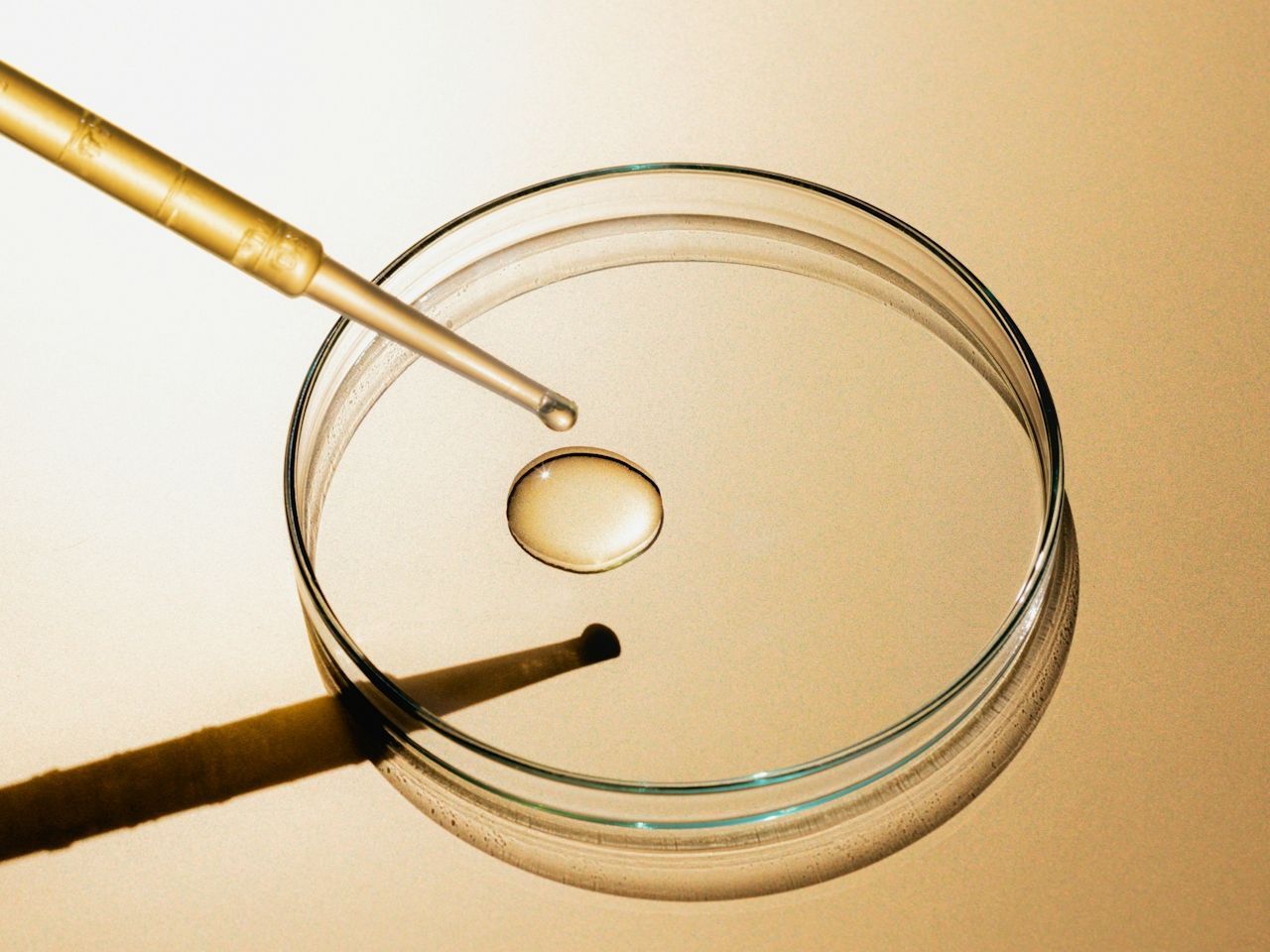
Exosomes
Perhaps the most important breakthrough in stem cell research isn't about the cells themselves, but what they release: exosomes. These nanoparticles are packed with proteins, lipids, and genetic material that cells use to communicate with each other.
Many researchers now believe exosomes are the primary way that stem cells exert their healing effects—by sending instructions to damaged tissues rather than replacing cells directly.
Exosomes offer several advantages over whole-cell treatments:
- No risk of tumor formation
- Better storage stability
- Lower immune rejection risk
- Ability to cross barriers cells cannot (including the blood–brain barrier)
These benefits have sparked a wave of exosome-based therapies for orthopedic injuries, neurological conditions, skin rejuvenation, and hair restoration. Many clinics now offer exosome treatments as alternatives to full stem cell procedures. As research advances, many believe exosomes represent the next evolution in regenerative medicine—potentially offering safer, more controllable therapies than whole-cell approaches.
WHERE STEM CELLS ARE MAKING AN IMPACT
Stem cells are being studied—and in some cases already used—as powerful tools to repair, regenerate, and modulate the body’s healing systems. Their ability to reduce inflammation, promote cellular regeneration, and even reshape immune responses makes them uniquely versatile.
Orthopedic Injuries and Joint Repair
This is perhaps the most advanced and widely applied use of stem cells today.
MSCs are being injected into joints and damaged tissues to encourage repair of cartilage, tendons, ligaments, and even intervertebral discs. In cases of osteoarthritis—especially in the knees and hips—stem cell injections are being used to slow degeneration and reduce pain. Athletes recovering from ACL tears, rotator cuff injuries, or chronic tendonitis are increasingly turning to stem cells as an alternative to invasive surgeries.
Many report decreased pain, improved mobility, and faster recovery. While not a cure-all, regenerative orthopedic care using stem cells is quickly moving from experimental to mainstream.
Neurological Disorders
Stem cells offer a glimmer of hope for conditions where there’s traditionally been very little. Diseases like Parkinson’s, multiple sclerosis, ALS, and spinal cord injuries involve the breakdown or dysfunction of neurons—cells that don’t naturally regenerate. Stem cells—especially neural and mesenchymal types—are being studied for their ability to reduce inflammation in the brain and spinal cord, promote repair of damaged neural tissues, and in some cases, form new neuron-like cells.
In stroke recovery trials, patients receiving stem cell infusions have shown measurable improvements in motor function. In multiple sclerosis, early studies suggest stem cells may help "reset" the immune system and reduce flare-ups. This is still early-stage science but for neurological conditions with few options, the potential is enormous.
Cardiovascular Repair
After a heart attack or in cases of heart failure, parts of the heart muscle are damaged or die due to lack of blood flow. That damage is usually permanent. But studies using stem cells—especially autologous (from your own body) and umbilical cord-derived MSCs—have shown the ability to improve cardiac function, encourage growth of new blood vessels (angiogenesis), and reduce scar tissue in the heart muscle.
Patients in some trials have demonstrated better heart output, less fatigue, and improved quality of life. While not yet a standard of care, stem cell therapy could one day be part of the toolbox for repairing damaged hearts.
Autoimmune and Inflammatory Conditions
Autoimmune diseases are driven by an overactive or misdirected immune system—your body attacking itself. Stem cells, particularly MSCs, have a unique ability to “calm” immune activity and promote tolerance, which is why they’re being used to treat conditions like Crohn’s disease, lupus, rheumatoid arthritis, and psoriasis.
In several clinical trials, patients who didn’t respond to traditional therapies showed reductions in inflammation, fewer flare-ups, and improved symptom control after receiving MSC therapy. This area holds promise for individuals who live with constant inflammation and have exhausted conventional treatments.
Eye Disease
The eye is small and less likely to attack transplanted cells, implants, or foreign material, which lowers the risk of inflammation or rejection—making it an ideal place to test regenerative therapies.
In cases of macular degeneration, retinitis pigmentosa, or corneal damage, stem cell-derived retinal or epithelial cells are being used to regenerate or replace damaged tissue. In several clinical trials, patients who were losing vision regained some functional eyesight after treatment—an outcome once thought impossible.
It’s still early, but stem cells may play a central role in restoring sight in the years to come.
Wound Healing and Tissue Regeneration
MSCs, delivered topically or via injection, help accelerate healing by reducing inflammation, stimulating collagen synthesis, and promoting the formation of new blood vessels. This makes them especially effective for burns, diabetic foot ulcers, radiation wounds, and other hard-to-heal injuries.
Unlike conventional treatments, stem cells don’t just close wounds—they help rebuild the underlying tissue, improving skin quality and reducing scarring. Clinical trials have shown faster recovery times and better long-term outcomes in both acute and chronic wound care. This is one of the most validated, high-impact uses of stem cells already gaining traction in hospitals and advanced care centers.
Cancer
Stem cells have long played a role in treating blood cancers. Bone marrow transplants for conditions like leukemia, lymphoma, and multiple myeloma involve hematopoietic stem cells that replenish the immune system after high-dose chemotherapy.
Now, researchers are going further by developing genetically modified stem cells that can target cancer cells more precisely, or repair tissue damaged by aggressive treatments.
There’s also interest in using iPSCs to create “off-the-shelf” immune cells or tumor-targeting cells tailored to a patient's biology. While still experimental, this approach could one day become part of personalized cancer therapy.
Skin and Hair Rejuvenation
In skincare, MSCs and perinatal stem cell derivatives are used to boost collagen, improve elasticity, and reduce signs of aging like fine lines, hyperpigmentation, and dullness. These therapies often pair with microneedling or laser treatments, using stem cell-conditioned media or exosomes to enhance results.
For hair, stem cell injections—typically MSCs or their secreted factors—aim to reactivate dormant follicles, improve scalp health, and increase hair density. While results vary, early studies show real promise, especially in early-stage hair thinning.
These treatments are already offered at advanced longevity clinics and are quickly becoming part of high-end regenerative protocols.
Anti-Aging and Longevity
This is where the line between medicine and wellness starts to blur—and where a lot of interest (and hype) lives.
Whole-body stem cell infusions, often using umbilical or placental MSCs, are being offered at longevity clinics around the world. Proponents claim benefits like better energy, enhanced immune function, reduced joint pain, and even younger-looking skin. Some even suggest it can lower biological age markers like inflammation, DNA methylation, and telomere attrition.
Much of the data is anecdotal or unpublished. But the early science—especially around immune rejuvenation and systemic inflammation reduction—is intriguing. The next 5–10 years will tell us much more.
WHERE THE SCIENCE IS GOING
Despite decades of work, stem cell research is still in its relative infancy—and yet the horizon is dazzling. Scientists around the world are pushing the boundaries of what’s possible, and the next decade could reshape how we think about disease, repair, and even aging itself. Here are seven areas where stem cell science is headed.
1. Personalized Regenerative Medicine
Imagine getting a new knee, made not of metal or plastic—but made from your own cells. That’s the goal of personalized regenerative medicine. By using a patient’s own stem cells (often through induced pluripotent stem cells, or iPSCs), researchers are working to grow customized replacement tissue—from cartilage and bone to heart valves, corneas, even entire organs.
Because the tissue is genetically matched, there’s no risk of immune rejection. And unlike donor transplants, there’s no waiting list. Clinical trials are already underway to regrow tracheas, bladders, and skin grafts using stem cell scaffolds. Eventually, we may be able to regrow what we lose—organ by organ.
2. Stem Cell Banking
Once seen as a niche idea, cord blood banking is now mainstream among forward-thinking parents. Umbilical cord blood and tissue are rich in hematopoietic and mesenchymal stem cells, which can be cryopreserved at birth and stored for potential future use. These cells can treat over 80 diseases today—including leukemia, lymphoma, and various immune disorders—and may play a role in tomorrow’s regenerative therapies.
Private companies now offer long-term storage plans, and some even allow for collection of dental pulp stem cells or adipose-derived cells later in life.
3. CRISPR + Stem Cells
What if we could not only regenerate tissue but correct its DNA first? That’s the vision behind combining stem cell therapies with gene editing tools like CRISPR.
Scientists are experimenting with editing defective genes inside stem cells before using them to repair tissues or organs. One promising application is in inherited diseases—like sickle cell anemia, cystic fibrosis, or muscular dystrophy. By correcting the faulty gene inside a patient’s own cells, reprogramming them into iPSCs, and differentiating them into the needed tissue, we could create perfectly healthy, personalized replacements.
4. Brain and Spinal Cord Repair
The brain has long been considered untouchable. Neurons don’t regenerate. Nerve damage is permanent. But that narrative is starting to change.
Stem cells—particularly neural stem cells and MSCs—are now being tested in human trials for spinal cord injuries, stroke, ALS, and even neurodegenerative diseases like Parkinson’s and Alzheimer’s. These cells may help by reducing inflammation, replacing lost neurons, or creating an environment more conducive to healing.
In spinal cord injury trials, patients have shown partial recovery of motor function. In stroke recovery studies, some regain strength and speech faster than expected.
We’re a long way from full cures—but the door is opening.
5. Stem Cell-Derived Organoids
Organoids are miniature, lab-grown versions of real human organs—cultivated from stem cells. They aren’t full-size organs, but they mimic their structure and function on a small scale.
Today, scientists have created brain organoids, gut organoids, kidney and liver organoids, and even beating clusters of heart tissue. These are already being used to test new drugs, study diseases, and model complex interactions without relying on animal testing. In the future, they may serve as the blueprint for building full-sized, transplantable organs—solving one of medicine’s greatest bottlenecks.
6. Autism Spectrum Disorder (ASD)
Though not yet FDA-approved, stem cell therapy is being studied as a potential treatment for autism—particularly using umbilical cord-derived mesenchymal stem cells (MSCs).
Researchers believe some forms of autism may involve chronic brain inflammation and immune dysfunction. Because MSCs are known to calm immune responses and reduce inflammation, they’re being tested for their ability to ease core symptoms. Early trials—mostly outside the US—have shown encouraging signs: improved communication, social engagement, and reduced repetitive behaviors, especially in children with inflammatory markers. But studies are small and results are inconsistent.
This remains an experimental therapy, and major autism organizations urge caution. Still, the potential is real—and may offer new hope for families as research continues.
7. Stem Cells and Aging
Here’s one of the boldest ideas in longevity science.
Aging is, at least in part, a stem cell problem.
As we grow older, our stem cells become fewer in number, less active, and more prone to dysfunction. Some researchers believe that replenishing or rejuvenating stem cells could reverse elements of biological aging—restoring immune function, improving tissue repair, and potentially extending healthspan.
Companies like Altos Labs (backed by Jeff Bezos) and Harvard’s Sinclair Lab are exploring how stem cell reprogramming—essentially turning back the cellular clock—could erase signs of aging in cells, and eventually in entire organisms.
While still theoretical, early experiments in mice and primates show potential.
WHAT’S ACTUALLY AVAILABLE RIGHT NOW?
FDA-Approved in the United States
These are legitimate, regulated therapies:
- Bone marrow transplants using hematopoietic stem cells (HSCs) for leukemia, lymphoma, and blood disorders like sickle cell anemia
- Umbilical cord blood transplants for certain immune or metabolic conditions
- Some orthopedic applications using autologous (your own) bone marrow or fat-derived stem cells in specific use cases under FDA’s HCT/P regulations
Most of these are covered by insurance when used for approved indications.
Experimental But Legal in the United States
These are therapies being used in clinical trials or under strict “investigational” use:
- MSCs for joint repair, autoimmune conditions, or neurological diseases like MS, Parkinson’s, or ALS
- Intrathecal injections for spinal cord injuries or neurodegenerative diseases
- iPSC-based therapies (still mostly in academic settings, not commercial clinics yet)
You can access some of these by enrolling in clinical trials, often through academic hospitals.
Available Abroad—But Not US FDA-Approved
Here’s where things get grayer and pricier:
- Full-body stem cell infusions for “anti-aging” and immune rejuvenation
- Umbilical or placental MSC treatments for general wellness
- Intranasal or experimental delivery methods for brain-related disorders
- Autism spectrum therapies (mostly in Panama, Mexico, Eastern Europe)
Some of these may be legitimate—offered by real doctors in regulated countries, but this is a difficult area to verify, so tread carefully.
What Does Stem Cell Therapy Cost?
Here’s one of the least discussed, but most important parts of the stem cell story: cost.
You're not just paying for the stem cells themselves.
You’re paying for:
- Cell harvesting and processing (especially if cryopreserved)
- Lab expansion and purification
- Clinical expertise and administration
- Imaging or surgical support
- Post-treatment care and follow-up
Depending on the type of stem cell therapy, where it’s done, and what it’s treating, costs can range from:
- $0–$10,000 for FDA-approved uses like bone marrow transplants (often covered by insurance)
- $5,000–$20,000 for orthopedic injections or systemic infusions at private clinics
- $20,000–$100,000+ for full-body “rejuvenation” protocols at elite longevity clinics abroad
Most of these are not covered by insurance, unless the treatment is FDA-approved for a specific condition (like leukemia).
It’s also worth noting that many “stem cell” therapies in the aesthetic space (like facials or topical serums) use cellular extracts, not live stem cells. These treatments are usually less expensive—but also far less potent. Right now, most stem cell therapies are only accessible to the wealthy or well-connected. Cord blood banking alone can cost $2,000–$3,000 upfront, plus annual storage fees.
There’s hope that as the technology scales, costs will drop. But for now, regenerative medicine remains a highly uneven playing field—and often more accessible in theory than in practice.
WHAT ABOUT THE RISKS?
Stem cells are one of the most exciting frontiers in medicine—but they’re also one of the most misunderstood. While some therapies are safe, well-studied, and FDA-approved, many others are experimental, unregulated, or outright fraudulent. Here’s what you need to know before considering any stem cell treatment.
Immune Rejection
If you’re receiving cells from a donor, your immune system may recognize them as foreign and attack. This can trigger inflammation or, in serious cases, graft-versus-host disease. Using your own cells (autologous therapy) generally avoids this—but it’s not always possible or practical.
Tumor Formation
Pluripotent stem cells (like embryonic stem cells or iPSCs) carry a risk of uncontrolled growth. If not carefully prepared and guided, they can form teratomas—tumor-like masses that contain disorganized tissue. That’s why these therapies are mostly limited to clinical trials with strict oversight.
Infection and Procedural Complications
Like any medical procedure involving injections or infusions, there’s risk of infection, inflammation, bleeding, or nerve damage, especially if performed without proper sterile technique. Poorly handled or contaminated cell products have led to serious complications, including blindness and paralysis in past cases.
Unproven and Unregulated Clinics
Perhaps the most widespread risk is false hope sold by unlicensed or deceptive providers, often abroad but increasingly in the United States too. These clinics offer stem cell treatments for everything from chronic pain to autism to aging—without peer-reviewed evidence, proper safety protocols, or long-term data. They often charge tens of thousands of dollars for what is essentially an untested experiment.
The FDA has issued warnings about these operations, and many major medical organizations have called for tighter regulation.
Questions to Ask
If you're considering a stem cell therapy—no matter how mainstream or cutting-edge it sounds—ask:
- What type of stem cells are being used? MSCs? iPSCs? HSCs? Perinatal cells? The source matters.
- Are the cells autologous (from me) or allogeneic (from a donor)? This affects both effectiveness and risk.
- Is the treatment FDA-approved or part of a registered clinical trial? If not, why not?
- What evidence supports this treatment? Ask to see published studies or trial results.
- Who is administering the therapy? Is it a licensed physician? Are they board-certified? What’s their experience?
- Where are the cells processed? Legitimate labs follow Good Manufacturing Practices (GMP). Anything less is a red flag.
Be Cautious with Medical Tourism
Many people travel abroad for stem cell procedures that aren’t legally allowed in their home country. Sometimes this works out. But often, it doesn’t.
You may be receiving poor-quality cells, treated by underqualified staff, with no follow-up care, and no legal recourse if things go wrong. The “stem cell” label is now slapped on everything from IV drips to facials to full-body infusions—many of them wildly overpriced, under-tested, or both.
A Clear Trajectory
Stem cells may represent one of the biggest medical revolutions of our time, and the future they promise is extraordinary. Conditions once considered permanent—from spinal cord injuries to neurodegenerative diseases—a glimmer of hope exists where there was none before.
But this revolution comes with important caveats. The gap between legitimate science and marketing claims remains wide. Access is uneven, costs are prohibitive for many, and regulation struggles to keep pace with innovation. The stem cell landscape resembles the Wild West in many ways—where breakthrough treatments exist alongside questionable therapies, where genius researchers share space with profit-driven marketers.
Still, the trajectory is clear. As research advances, costs decrease, and regulations mature, regenerative medicine will likely become an essential part of healthcare—not just for the wealthy or desperate, but for anyone seeking alternatives to traditional approaches.
For those considering these therapies today, proceed with knowledge and caution. Ask hard questions. Demand evidence. Work with legitimate practitioners. Be skeptical of miracle claims, especially when paired with premium price tags.
|
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

February 20, 2026

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026