Most people only think about their immune system when it’s already failing them. But it’s working for you around the clock—shaping how you feel, how fast you heal, and even how you age.
In The Daily Immunity Issue, we explored the foundations of a resilient immune system: the overlooked roles of sleep, gut health, movement, and mindset. We also broke down common myths, subtle immune disruptors, and what actually works to build long-term defense.
Didn’t catch it? You can still dive into the full issue. Catch up here.
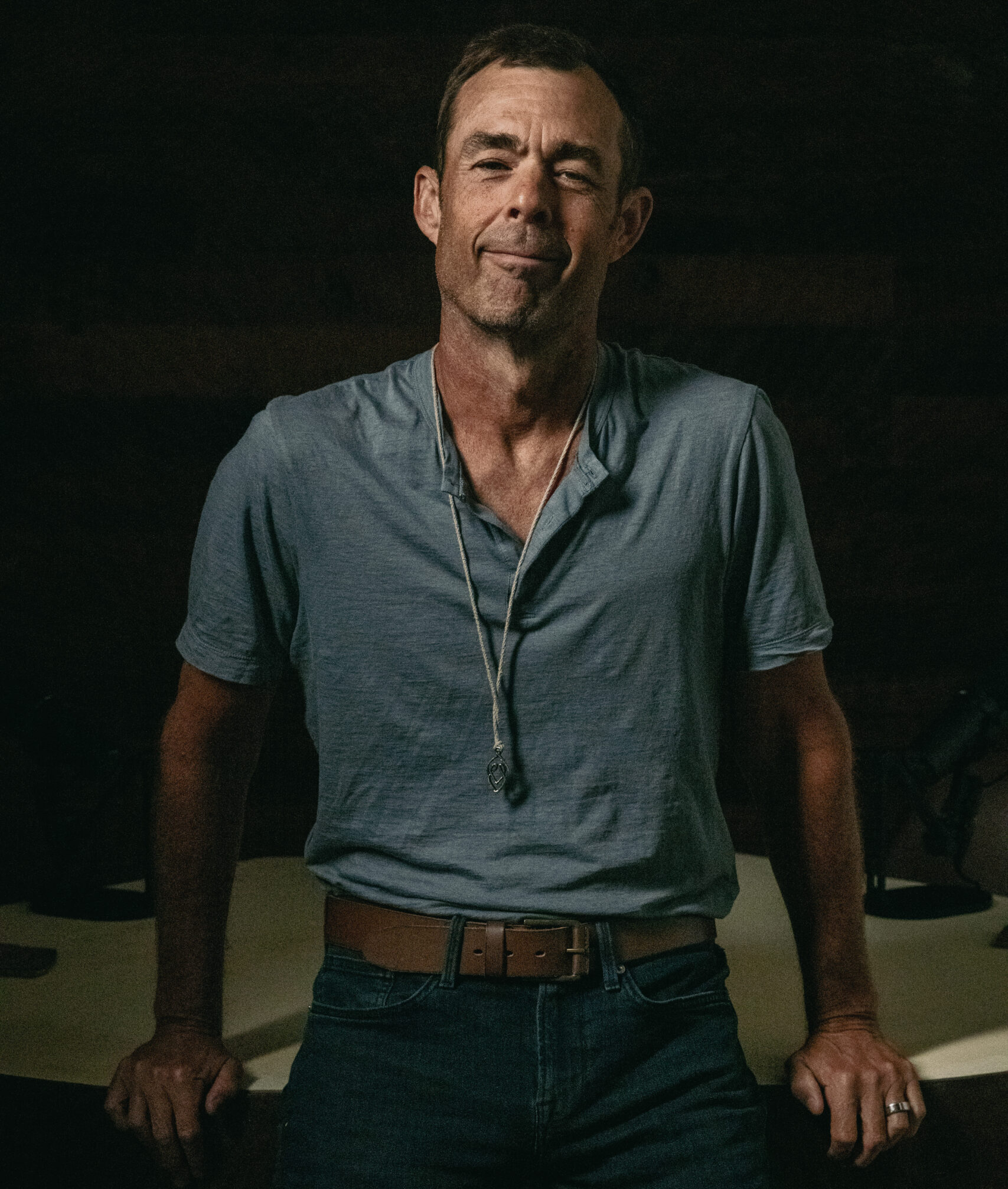
Today’s featured expert is Dr. David Perlmutter.
Dr. Perlmutter is a Board-Certified Neurologist and six-time New York Times bestselling author. He serves on the Board of Directors, is a Fellow of the American College of Nutrition, and currently serves as the Director of Neuroscience Research at Bryan Therapeutics.
Dr. Perlmutter received his MD from the University of Miami School of Medicine, where he was awarded the Leonard G. Rowntree Research Award. He serves as a member of the Editorial Board for the Journal of Alzheimer’s Disease and has published extensively in peer-reviewed scientific journals including Archives of Neurology, Neurosurgery, and The Journal of Applied Nutrition.
Lucky for us, he was game to tackle your biggest questions about daily immunity. His answers are clear, thoughtful, and genuinely useful.
Q. Why do some people never get sick, even when exposed to everything? Genetic luck? Lifestyle?
While genetics and chance play a role, one of the most clinically underappreciated factors is metabolic health. Metabolically healthy individuals (i.e., those with balanced blood sugar, low inflammation, good mitochondrial function, and optimal body composition) consistently exhibit stronger and more resilient immune function.
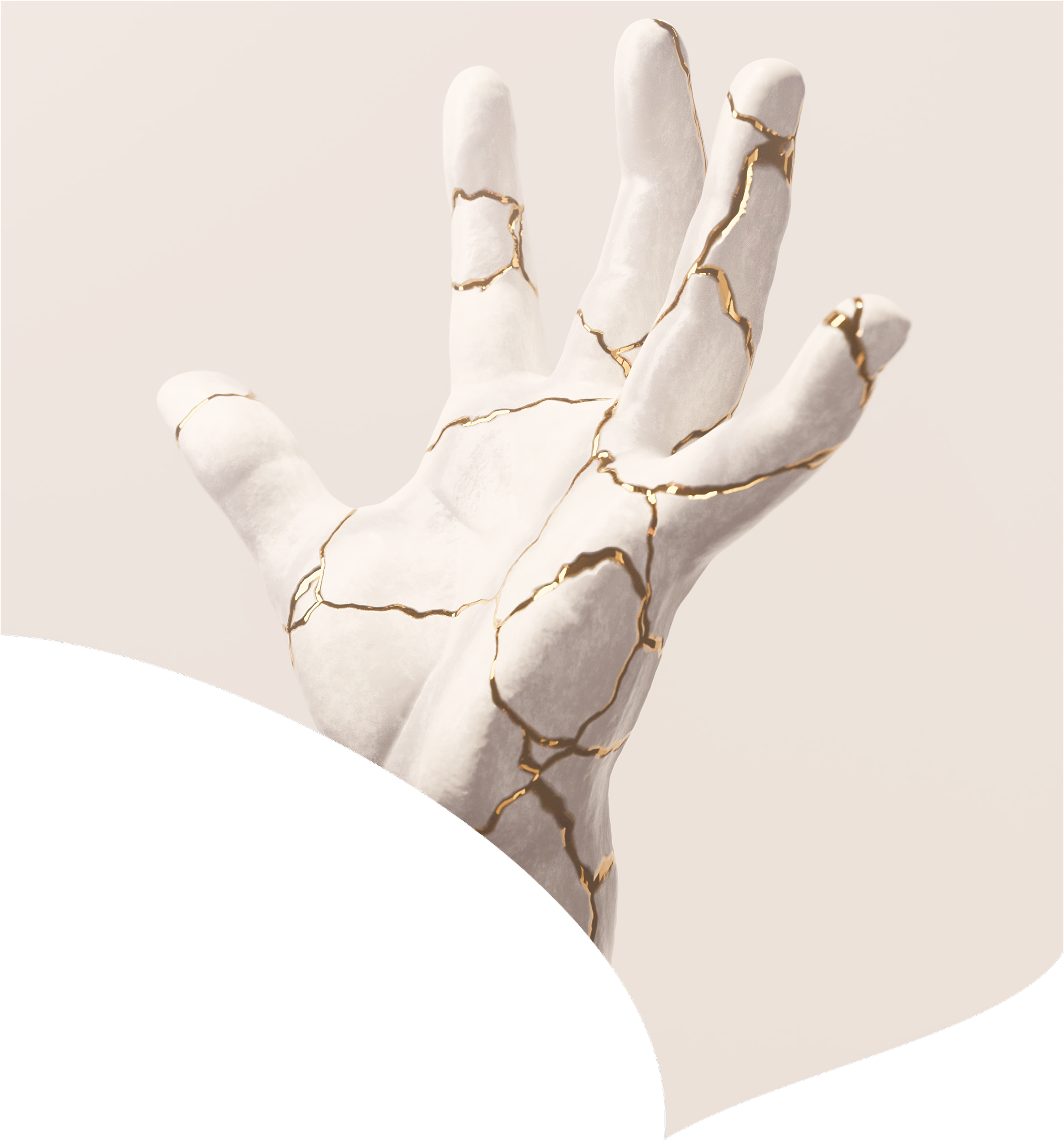
This critical relationship is now referred to as immunometabolism. This term underscores the deep interdependence between the immune system and metabolic function. Immune cells rely on specific metabolic pathways to function properly. When metabolic function is disrupted due to insulin resistance or obesity, immunity is compromised.
So, while some might attribute resistance to illness as “genetic luck,” the truth is that many people who rarely get sick are actively engaged in supporting their metabolic health through lifestyle choices like regular exercise, nutrient-dense diets, restorative sleep, and stress management. In turn, this supports stronger immunity and greater protection against infectious disease.
Q. What’s the single most underrated habit for long-term immune strength?
In my experience, exercise stands out above all. While commonly recognized for its benefits in weight control, cardiovascular fitness, and even brain health, the greater value of sustained physical activity lies in how profoundly it enhances metabolic health and, in turn, immune resilience.
Exercise improves mitochondrial function, increases insulin sensitivity, lowers chronic inflammation, and promotes hormonal balance. These effects cultivate an internal physiological state in which immune cells can function at their peak. Physical activity also supports lymphatic flow, which is critical for immune surveillance, and helps regulate the balance between pro-inflammatory and anti-inflammatory immune responses.
Numerous studies have demonstrated that regular, moderate exercise not only reduces the risk of chronic diseases but also lowers the incidence and severity of viral infections. This exemplifies the principles of immunometabolism in practice. By enhancing metabolism, exercise strengthens immune function.
It remains underutilized, perhaps because many people turn to supplements or immune-boosting remedies during flu season or when facing a new virus. However, true long-term immune resilience is cultivated gradually through movement. Whether through brisk walking, resistance training, cycling, or swimming, sustained physical activity is one of the most powerful interventions for maintaining a strong and responsive immune system over time.
Q. What are the top 3 biomarkers to assess someone’s immune health today?
An immunologist might answer this by highlighting specific immune markers related to the various cell types that regulate immune responses. However, given what we know about the connection between metabolism and immunity (immunometabolism) the most insightful biomarkers reflect both systems simultaneously.
Here are 3 examples of key markers I would consider most insightful:
1. Insulin Sensitivity (Fasting Insulin or HOMA-IR)
Insulin resistance is a central contributor to chronic inflammation and impaired immune function. Elevated fasting insulin or HOMA-IR scores indicate metabolic stress, which interferes with immune cell function, promotes inflammatory cytokine production, and increases vulnerability to infection. In contrast, enhanced insulin sensitivity allows for more efficient energy utilization by immune cells and supports more balanced immune responses.
2. High-Sensitivity CRP (hs-CRP)
This is a reliable marker of systemic inflammation. Chronic low-grade inflammation, often driven by poor metabolic health, disrupts immune regulation and accelerates immune aging, sometimes referred to as "inflammaging." Lower hs-CRP levels tend to reflect a more stable and regulated immune environment and are associated with better overall health outcomes.
3. Ratio of Triglycerides to HDL
This clinically practical and informative metric reflects both lipid metabolism and insulin sensitivity. A high ratio has been associated with reduced immune surveillance and elevated inflammatory signaling. A lower ratio suggests more efficient metabolic function and, by extension, a more resilient and well-regulated immune system.
All of these serve as proxies for immune readiness, and optimizing them means providing the immune system the foundation it needs to function best.
Importantly, all 3 of these can be improved through lifestyle intervention.
Catch Dr. David Perlmutter at Eudēmonia Summit
Join us in person November 13–16 at West Palm Beach and ask your own questions of America’s Neurologist™.
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

February 20, 2026

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026