In our last stem cells issue, we explored the future of regenerative medicine—how stem cells are reshaping what it means to heal, recover, and even age. We broke down the types of stem cells, their therapeutic uses, the emerging research, and the risks and realities behind the hype.
Missed it? You can still catch up on Part 1 of The Stem Cells Issue.
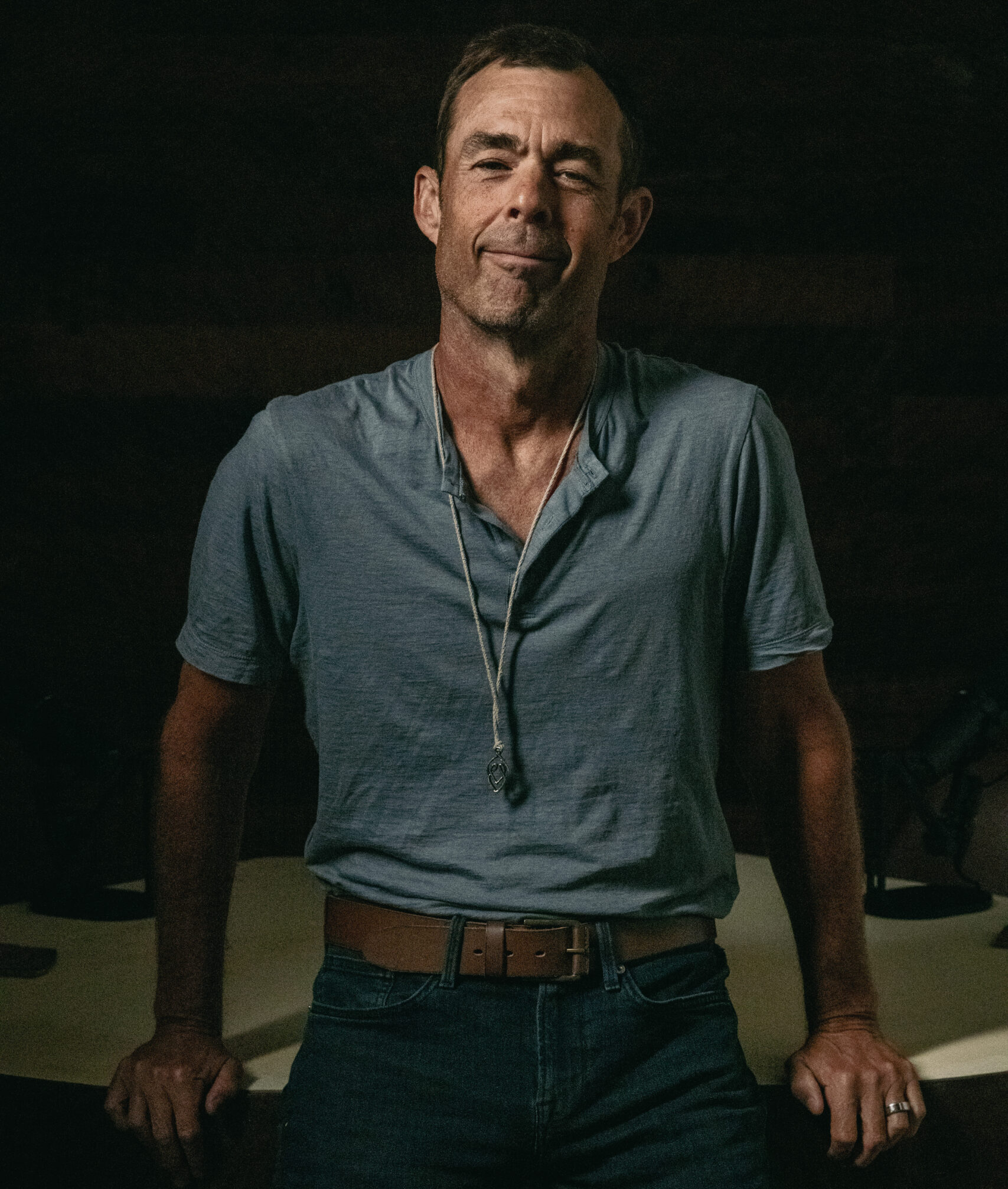
But when it comes to the next frontier—how to naturally enhance your body’s own stem cell production—you had more questions. So we brought them to an expert—Christian Drapeau, MSc.
Christian is a neurophysiology scientist and a true pioneer in the world of stem cell science. More than two decades ago, Christian was one of the first to propose that adult stem cells are the body's natural repair system—an idea that's now foundational to regenerative medicine.
As the founder and Chief Science Officer of STEMREGEN, Christian's mission is to discover natural ways to stimulate stem cell production, especially through plant-based compounds. His research has helped shape a new wave of stem cell-enhancing therapies, and he’s built a community of over 700,000 people eager to learn how we can activate our body's own healing power.
QUESTION 1: What’s the most misunderstood thing about stem cells?
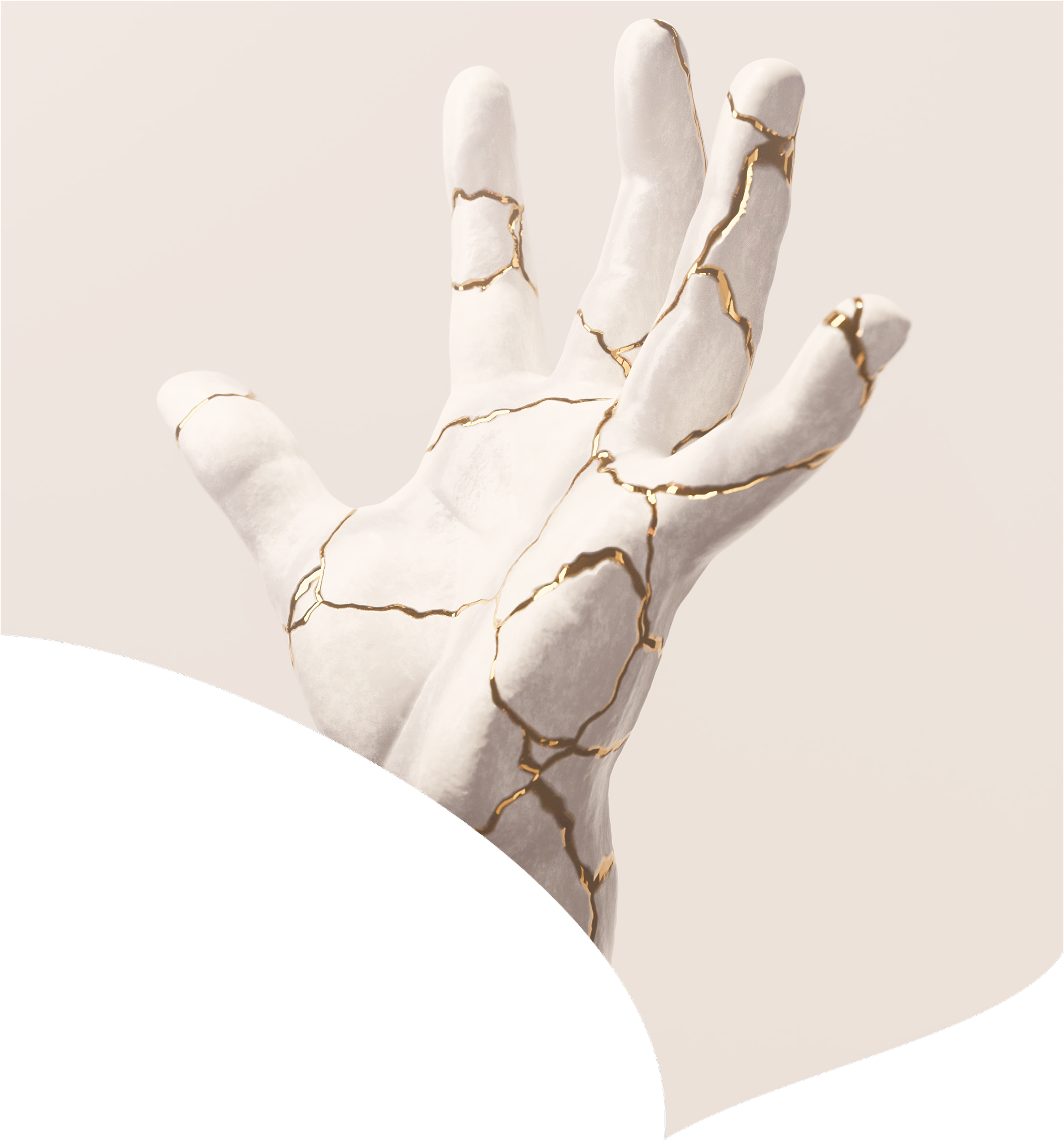
Stem cells are often viewed solely as a medical treatment—something you receive through an injection. But in reality, they are an essential part of your body’s innate repair system, much like the immune system is essential for fighting infections. Just as you rely on your immune cells to defend against an infection, you rely on your stem cells to repair and regenerate tissues throughout your life. These cells are active every day, playing a critical role in maintaining health and vitality as you age.
The age-related decline in the number of circulating stem cells is a fundamental cause of disease formation. Significant health benefits can be achieved simply by supporting your body’s own stem cell function—through lifestyle practices such as fasting and regular physical activity, or by using plant-based compounds that have been scientifically shown to enhance stem cell activity.
QUESTION 2: What breakthrough in stem cell research are you most excited about right now?
I’m currently following two major breakthroughs that could redefine how we think about stem cells and their role in health and healing.
The first is the discovery of MUSE cells, which stands for Multilineage Stress-Enduring stem cells. These cells, identified just a few years ago, may prove to be the most powerful stem cells in the human body. What makes them so remarkable is their ability to survive extreme stress and naturally migrate to damaged tissues—where they then differentiate and repair. They’re potent and safe. And because they exist in adult tissues, they can be sourced from the patient’s own body, eliminating concerns around immune rejection, contamination, and disease transfer. The main challenge right now is that they’re difficult to isolate. But once efficient extraction methods are developed, MUSE cells could become the gold standard in stem cell therapy.
To appreciate the significance of this, it helps to understand the limitations of current stem cell sources. For instance, umbilical and placental stem cells are young and highly potent, but they come with risks—such as immune sensitivity, contamination, disease transfer and limited availability. Fat-derived stem cells are safer and easier to obtain but are generally less potent. And while VSELs (Very Small Embryonic-Like stem cells) show great promise in terms of potency and safety, they’re often dormant and still lack robust clinical evidence.
MUSE cells, on the other hand, offer a rare combination of potency, safety, and autologous availability—potentially making them the most ideal stem cell type we’ve discovered to date.
The second breakthrough is more conceptual but equally transformative: the realization that stem cells are the body’s own repair system. For a long time, stem cell therapy was seen as something external—you’d go to a clinic and get an injection. But we now understand that every human already has stem cells circulating in their body, playing a central role in tissue repair and regeneration. This ongoing process helps maintain our organs and tissues throughout life. In fact, one of the main reasons we develop chronic diseases as we age is the natural decline in the number of circulating stem cells.
This insight changes everything. It shifts the focus from stem cells as a one-time therapy to stem cells as a daily pillar of health. It opens the door to strategies aimed at supporting and enhancing the body’s own regenerative capacity. When this understanding becomes mainstream in medicine, it will fundamentally change how we approach aging, disease, and longevity. So far, data suggests that daily plant-based stem cell enhancers that trigger the release of one’s own stem cells (a process referred to as Endogenous Stem Cell Mobilization)—coupled with treatments using adipose-derived stem cell injections that can be done in the United States—could be an effective strategy for optimal health and longevity.
QUESTION 3: What's the difference between stem cells from umbilical cords or placentas and stem cells from adults?
To answer this question, it’s helpful to understand the three main attributes that define the quality and usefulness of any stem cell source: safety, potency, and availability.
Safety is primarily influenced by the origin of the cells and the risk of contamination during collection or processing. Potency refers to the cells’ ability to regenerate and repair tissues, which determines the therapeutic impact. And availability speaks to how easily and consistently the cells can be sourced.
Umbilical and placental stem cells are considered highly potent and youthful, making them an attractive option from a clinical perspective. However, they come with limitations. Their availability is restricted by the number of births occurring in facilities equipped for proper, sterile collection. There’s also a small but real risk of contamination if the cells are mishandled during harvesting or storage. In addition, because these are donor cells, there’s a minimal risk of transmitting genetic conditions to the recipient. That said, when sourced from reputable clinics that follow strict protocols, these risks remain very low, and treatments are generally considered safe.
On the other hand, autologous stem cells—those derived from an individual’s own blood, bone marrow, or fat—are widely regarded as safe, since there’s no risk of immune rejection or transmission of disease. While some debate remains about whether they are as potent as umbilical or placental stem cells, numerous studies and clinical outcomes suggest they can be highly effective. A major advantage is that they are unlimited in supply, as they can be collected from the individual at any stage of life with minimal risk of contamination.
Today, the use of umbilical and placental stem cells is rising in popularity, largely because of their convenience. They are pre-packaged, ready to use, and typically less labor-intensive than the procedures required to extract a patient’s own stem cells. Their increasing popularity is driven by ease of use and lower procedural costs, though for many patients, autologous options may still be preferable depending on the clinical context and desired outcome.
QUESTION 4: I know two people who have had stem cell injections and developed serious infections.
What are the risks, and how can we manage them?
Like any medical procedure that involves an injection into the body, stem cell therapy carries a small risk of infection. The most reported adverse effect associated with stem cell injections to date is systemic infection, usually resulting from bacterial contamination during collection, handling, or administration of the cells. While this risk is rare, it’s important to take it seriously.
To put it into perspective, the rate of systemic infection following surgery is approximately 0.5 to 1%, with higher rates in more complex or high-risk procedures. Similarly, the risk of infection with stem cell therapy is largely tied to the source of the cells and the standards of the clinic performing the procedure.
The highest risk is associated with allogeneic stem cells—those derived from sources like umbilical cord, placenta, or Wharton’s jelly. If these cells are not collected, stored, or transported under strict sterile and temperature-controlled conditions, contamination becomes more likely. That’s why choosing a qualified provider who works with high-quality, properly handled cell sources is absolutely essential.
On the other hand, therapies that use your own stem cells (autologous therapy) carry far less risk of infection, as the body is naturally adapted to its own cells, and there’s no risk of immune rejection or donor contamination.
The safest way to approach stem cell therapy is to ensure you’re working with a reputable medical professional who sources stem cells from trusted, properly regulated facilities. Avoid treatments that seem too inexpensive or unverified. Cutting corners in this area can carry significant risk. When done right, stem cell therapy is not only powerful—it’s also very safe.
QUESTION 5: Do you believe full organ regeneration using stem cells will be possible in our lifetime?
Full organ regeneration using stem cells is no longer a concept confined to science fiction. However, whether it becomes a widespread clinical reality in our lifetime depends on how we define both “our lifetime” and “full regeneration.” Remarkable progress has already been made—scientists have successfully grown organ-like structures (organoids), such as miniature brains, livers, kidneys, and intestines in laboratory settings. In some studies, researchers have even demonstrated the possibility of growing a complete heart in a lab environment. Using organic scaffolds, stem cells can be guided to form cartilage and, with further development, entire functional organs.
One of the major hurdles that remains is the ability to guide stem cells to develop the full complexity of an organ’s structure, including its microcirculation and the intricate cellular architecture seen in organs like the liver, kidney, and brain. These elements are crucial for long-term viability and function post-transplantation.
For younger generations, it’s quite likely that full or partial organ regeneration will become clinically available for certain organs within their lifetime. For those in older generations, the future is more likely to bring highly advanced cellular therapies, bioengineered scaffolds, and hybrid bioartificial organs—combinations of biological tissue and synthetic materials that restore function. While fully regenerating a complex, custom-built organ from a patient’s own stem cells may still be decades away from routine clinical use, the foundational science and technological advances to make it possible are already in motion.
|
Disclaimer: This newsletter is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.

February 14, 2026

February 6, 2026

January 31, 2026

January 23, 2026
January 16, 2026

January 9, 2026

January 2, 2026